Abstract
This case report utilized a patients natural teeth as provisional restorations supported by immediately placed implants to provide a seamless transition from hopeless teeth to implant supported restorations.
Introduction
Patients facing the unexpected loss of a tooth in the esthetic zone in an otherwise healthy dentition may feel psychologically distressed. The placement of an implant into a fresh extraction socket followed by an immediate provisional restoration supported by the implant can help alleviate an upsetting experience. The utilization of a patient׳s own teeth can further provide a seamless transition from hopeless teeth to implant supported restorations.
Immediate implant placement and immediate provisionalisation (IIPIP) of a single anterior tooth have been documented to have high success rates ranging from 93.5% to 100% [1] , [2] , [3] and [4] . The results are comparable to implants placed in healed sites with immediate provisionalisation [5] and [6] or delayed loading approach [7] and [8] with reported success rates of 100% and 97% respectively.
In addition to shortened treatment time and smooth conversion, the flapless approach of IIPIP which maintains the blood supply to the buccal bone plate could help minimize changes in the facial–palatal contour [9] , [10] and [11] . Although bone remodeling cannot be halted by the immediate placement of the implant [12] and [13] , the immediate provisionalisation acts as a scaffold to support the existing soft tissues from flattening [1] and [11] .
Various techniques have been described for the construction of implant supported provisional restorations with the aim to support the peri-implant tissues [1] , [9] and [11] . Provisional shells made with auto-polymerizing acrylic resin are the most commonly prescribed methods, however, much chair-time is required to accurately reproduce the interproximal contacts and identify the location of the cervical margin. Furthermore, the provisional materials are vulnerable to staining and fracture with time.
This case report utilized a patient׳s natural teeth as provisional restorations supported by the immediately placed implants.
Case report
A twenty-six year old male patient was referred for the management of the symptomatic maxillary left central and lateral incisors. The incisors were diagnosed with external root resorption due to history of trauma. The long-term endodontic prognoses were assessed to be poor (Figs. 1 a, b and 2 ).
|
|
|
Fig. 1. (a) Labial view of the pre-operative clinical condition. (b) Palatal view of the pre-operative clinical condition. |
|
|
|
Fig. 2. Pre-operative periapical radiograph showing external root resorption of maxillary left central and lateral incisors. |
Cone beam computed tomography (CBCT) revealed the presence of buccal plate and the patient was treatment planned to receive immediate implant placement and immediate provisionalisation for both the central and lateral incisors (Fig. 3 a and b). The IIPIP procedures for the two teeth were performed on two separate visits to maintain the integrity of interproximal bone. The IIPIP of lateral incisor was carried out six weeks following IIPIP of central incisor when the peri-implant tissues have stabilized (Fig. 4 a and b).
|
|
|
Fig. 3. (a) CBCT showing intact buccal plate and a 3.5 mm Nobel Active implant of 15 mm length was planned for the replacement of central incisor. (b) CBCT showing intact buccal plate and a 3 mm Nobel Active implant of 15 mm length was planned for the replacement of lateral incisor. |
|
|
|
Fig. 4. (a) Labial view of soft tissue healing 6 weeks after IIPIP of central incisor. (b) Screw access hole on the palatal surface of implant supported natural crown of left central incisor. |
Following local anesthesia, sharp dissection of the supracrestal fibers with a 15c scalpel blade was performed and the tooth was removed carefully with extraction forceps (Fig. 5 a and b). The socket was thoroughly debrided with a surgical excavator and rinsed with saline. The integrity of the buccal wall was verified (Fig. 5 c). Two 15 mm threaded and textured implants with diameters of 3.5 mm and 3 mm (Nobel Active, Nobel Biocare) were placed at central and lateral incisor sites respectively on two separate visits. The implants were placed toward the palatal aspect of the extraction sockets to a depth of 3–4 mm from the free gingival margin (Fig. 6 a and b). A minimum torque value of 30–35 N cm upon implant placement was confirmed prior to immediate provisionalisation.
|
|
|
Fig. 5. (a) Removal of maxillary lateral incisor with forceps. (b) Extracted maxillary left lateral incisor showing extensive area of external root resorption. (c) Presence of buccal bone verified at 3 mm below the free gingival margin at extracted site. |
|
|
|
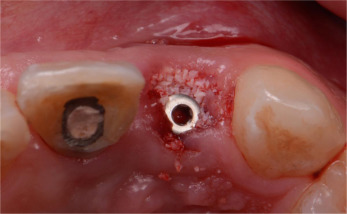
Fig. 6. (a) Implant (3.5 mm×15 mm) placed at extracted socket of central incisor. (b) Implant (3 mm×15 mm) placed at extracted socket of lateral incisor. |
The anatomical crown of the extracted tooth was sectioned off and the screw access hole was created on the palatal surface of the crown (Fig. 7 ). A screw retained provisional abutment was placed onto the implants. The natural crown was steam cleaned, treated, and connected to the temporary abutment with flowable composite resin intra-orally with an aid of a position index (Fig. 8 a and b). The connected provisional restoration was then removed from the implant and composite resins were used to contour the sub-gingival portion (Fig. 9 a and b). It is crucial the subgingical contour supported the peri-implant tissue.
|
|
|
Fig. 7. Screw access hole created on the palatal surface of the sectioned anatomical crown of lateral incisor. |
|
|
|
Fig. 8. (a) Provisional crown was etched and primed. (b) The crown was repositioned with an aid of a matrix. |
|
|
|
Fig. 9. (a) The crown connected to the temporary abutment. (b) Composite resin used to contour the tissue surface. |
Upon completion of the screw retained provisional restoration, a tall, flat-contoured healing abutment was placed onto the implant prior to the placement of bone graft materials. The healing abutment allowed the grafting materials to be placed and packed against it at the same time prevented the excess from entering the screw channel. A xenograft bone graft material (Bio-Oss, Geistlich Pharma AG) was used to fill the gap between the implant and the buccal wall as well as the space above up to the most coronal aspect of the free gingival margin (Fig. 10 ). The healing abutment was then removed, leaving the bone graft material intact. The prepared provisional restoration was subsequently screwed onto the implants and the access was sealed with a temporary material (Cavit temporary filling materials, 3M, ESPE). The occlusion was adjusted to clear all static and dynamic occlusal contacts (Fig. 11 ). The technique resulted in minimum alteration of the patient׳s esthetics (Fig. 12 ).
|
|
|
Fig. 10. Bone grafting materials packed against the healing abutment. |
|
|
|
Fig. 11. Occlusion cleared of any static and dynamic contacts. |
|
|
|
Fig. 12. Post-operative clinical view of IIPIP of left lateral incisor on the day of surgery (IIPIP of central incisor was completed 6 weeks prior). |
Discussion
Tooth removal results in marked reduction in buccal–lingual alveolar bone width [14] and [15] . Araujo and Lindhe showed that the reduction of the dimension of an extraction site was due to the replacement of bundle bone with woven bone from the inner portion of the socket and the resorption of the outer and crestal portions of the buccal–lingual socket walls [16] .
Various techniques have been proposed to place implants immediately following extraction [17] . Assessment of the morphology of the pre-extraction socket is essential. Elian et al. classified the extraction site based on the presence or absence of the labial and interproximal bone, and its overlying gingival tissue and papilla surrounding the compromised tooth to be extracted [18] . When a socket is not compromised, described as a type I socket, the use of bone graft coupled with flapless surgery can help limit the amount of buccal contour change [11] , [19] and [20] . The grafting materials are then contained by the provisional restoration.
The use of a position matrix is an effective method to reposition the sectioned natural crown back to its pre-extracted spatial position. The use of the patient׳s own tooth simplified the provisionalisation procedure as no modification was required for cervical margins and interproximal contacts. Furthermore, the tissue response to the patient׳s own tooth could be expected to be more superior than other provisional materials, which tends to promote plaque accumulation if it is porous or unpolished.
Conclusion
The patient׳s extracted teeth can be used as provisional restorations following immediate implant placement for a seamless transition from hopeless teeth to implant supported restorations.
References
- [1] J.Y. Kan, K. Rungcharassaeng, J.L. Lozada, G. Zimmerman; Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: a 2-to 8-year follow-up; Int. J. Oral Maxillofac. Implants, 26 (1) (2010), pp. 179–187
- [2] T. De Rouck, K. Collys, J. Cosyn; Immediate single tooth implants in the anterior maxilla: a 1-year case cohort study on hard and soft tissue response; J. Clin. Periodontol., 35 (2008), pp. 649–657
- [3] P. Palattella, F. Torsello, L. Cordaro; Two-year prospective clinical comparison of immediate replacement vs immediate restoration of single tooth in the esthetic zone; Clin. Oral Implants Res., 19 (2008), pp. 1148–1153
- [4] R. Crespi, P. Cappare, E. Gherlone, G. Romanos; Immediate versus delayed loading of dental implants placed in fresh extraction sockets in the maxillary esthetic zone: a clinical comparative study; Int. J. Oral Maxillofac. Implants, 23 (2008), pp. 753–758
- [5] L.F. Cooper, F. Raes, G.J. Reside, J.S. Garriga, L.G. Tarrida, J. Wiltfang, M. Kern, H. de Bruyn; Comparison of radiographic and clinical outcomes following immediate provisionalization of single-tooth dental implants placed in healed alveolar ridges and extraction sockets; Int. J. Oral Maxillofac. Implants, 25 (6) (2010), pp. 1222–1232
- [6] E. Andersen, H.R. Haanaes, B.M. Knutsen; Immediate loading of single-tooth ITI implants in the anterior maxilla: a prospective 5-year pilot study; Clin. Oral Implants Res., 13 (2002), pp. 281–287
- [7] E. Romeo, M. Chiapasco, M. Ghisolfi, G. Vogel; Long-term clinical effectiveness of oral implants in the treatment of partial edentulism. Seven-year life table analysis of a prospective study with ITI dental implant system used for single tooth restorations; Clin. Oral Implants Res., 13 (2002), pp. 135–143
- [8] L. Levin, P. Sadet, Y. Grossman; A retrospective evaluation of 1387 single-tooth implants: a six-year follow-up; J. Periodontol., 77 (2006), pp. 2080–2083
- [9] M. Degidi, D. Nardi, G. Daprile, A. Piattelli; Buccal bone plate in the immediately placed and restored maxillary single implant: a 7-year retrospective study using computed tomography; Implant Dent., 21 (1) (2012), pp. 62–66
- [10] A.M. Albiero, R. Benato, M. Degidi; Buccal plate regeneration with immediate post extraction implant placement and restoration: case reports; Int. J. Periodontics Restor. Dent., 34 (4) (2014), pp. e67–e72
- [11] D.P. Tarnow, S.J. Chu, M.A. Salama, C.F. Stappert, H. Salama, D.A. Garber, G.O. Sarnachiaro, E. Sarnachiaro, S.L. Gotta, H. Saito; Flapless post extraction socket implant placement in the esthetic zone: Part 1. The effect of bone grafting and/or provisional restoration on facial–palatal ridge dimensional change – a retrospective cohort study; Int. J. Periodontics Restor. Dent., 34 (3) (2014), pp. 323–331
- [12] M.G. Araújo, F. Sukekava, J.L. Wennström, J. Lindhe; Tissue modeling following implant placement in fresh extraction sockets; Clin. Oral Implants Res., 17 (6) (2006), pp. 615–624
- [13] M. Sanz, D. Cecchinato, J. Ferrus, E.B. Pjetursson, N.P. Lang, L. Jan; A prospective, randomized-controlled clinical trial to evaluate bone preservation using implants with different geometry placed into extraction sockets in the maxilla; Clin. Oral Implants Res., 21 (2010), pp. 13–21
- [14] F. Van der Weijden, F. Dell’Acqua, D.E. Slot; Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review; J. Clin. Periodontol., 36 (2009), pp. 1048–1058
- [15] W.L. Tan, T.L.T. Wong, M.C.M. Wong, N.P. Lang; A systematic review of postextraction alveolar hard and soft tissue dimensional changes in humans; Clin. Oral Implants Res., 23 (s5) (2012), pp. 1–21
- [16] M.G. Araújo, J. Lindhe; Dimensional ridge alterations following tooth extraction. An experimental study in the dog; J. Clin. Periodontol., 32 (2) (2005), pp. 212–218
- [17] C.H. Hammerle, S. Chen, T.G. Wilson; Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets; Int. J. Oral Maxillofac. Implants, 9 (Suppl.) (2004), pp. S26–S28
- [18] N. Elian, S.C. Cho, S. Froum, et al.; A simplified socket classification and repair technique; Pract. Proced. Aesthet. Dent., 19 (2) (2007), pp. 99–104
- [19] S.J. Chu, M. Salama, H. Salama, D.A. Garber, H. Saito, G.O. Sarnachiaro, D. Tarnow; The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets; Compend. Contin. Educ. Dent., 37 (2011), pp. 524–532
- [20] M.G. Araújo, E. Linder, J. Lindhe; Bio-Oss collagen in the buccal gap at immediate implants: a 6-month study in the dog; Clin. Oral Implants Res., 22 (l) (2011), pp. l–8
Document information
Published on 20/10/16
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?