Keywords
Pulmonary vein thrombosis;Optimum duration of DAPT;64-MDCT;Stent
The optimum duration of dual antiplatelet treatment (DAPT) with a thienopyridine drug (clopidogrel or prasugrel) and aspirin to prevent stent thrombosis after coronary drug-eluting stent placement remains uncertain. Some studies report the merits and demerits of extended treatment.
Continued thienopyridine treatment beyond one year after placement of a drug-eluting stent, compared with aspirin therapy alone, reduced the rates of stent thrombosis, myocardial infarction and cerebrovascular events. However, the rate of death from any cause was increased with continued thienopyridine treatment [1] ; [2]. Additionally, a significant increase in the risk of cancer-related death in patients receiving continuous DAPT, compared with aspirin therapy alone, was reported [1], indicating that we require a method to estimate the effects of antiplatelets drugs.
Palmerini et al. reported that patients treated with DAPT for longer than one year had a higher risk of mortality but a lower risk of myocardial infarction and stent thrombosis compared with patients treated with DAPT for six months or shorter and for one year. Patients treated with one-year DAPT had similar rates of mortality, myocardial infarction and stent thrombosis but higher rates of major bleeding compared with patients treated for six months or less [2].
More than a one-year treatment of DAPT results in injurious effects. When to stop or decrease the dose of the drug is a crucial problem. Additionally, whether pairing of aspirin and thienopyridine is best for any patient is unknown because how to assess the effects of the anticoagulants is unknown.
How to decide the optimum duration and how to choose the optimum antithrombotic drugs remain uncertain because the optimum assessment method for antithrombotic drugs remains unknown.
Since 2012, I have published many cases of pulmonary vein thromboses using 64-slice multidetector computed tomography (64-MDCT) [3]; [4]; [5]; [6]; [7]; [8]; [9] ; [10]. In 2014, I reported that 35 (61%) of 57 elderly patients with chest pain had pulmonary vein thromboses [4]. I reported that we could assess the resistance of antiplatelet therapies using 64-MDCT [9].
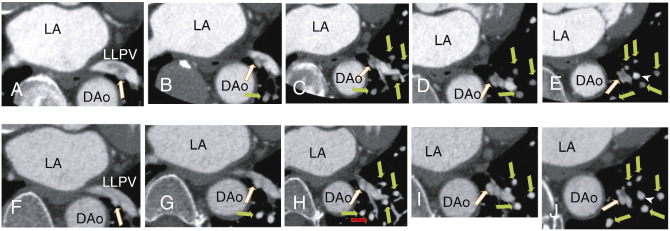
In this manuscript, a 64-MDCT scan showed that a 68-year-old male had thrombi in the left lower pulmonary vein (LLPV) and the branches of the LLPV (Fig. 1A to E). After three months of dabigatran therapy, the thrombus was dissolved almost entirely (Fig. 1F to J). In Fig. 1H, the red arrow indicates a newly appeared enhanced pulmonary vein that was not illustrated in Fig. 1C, indicating that dabigatran restored a collapsed pulmonary vein by dissolving the thrombus.
|
|
|
Fig. 1. An axial image demonstrating A: A thrombus in the left lower pulmonary vein (LLPV) as a defect of contrast enhancements (white arrow). B: The thrombus becomes smaller, indicating that one branch of the LLPV was occluded (white arrow), and the occluded small pulmonary vein was illustrated (green arrow). C to E: The occluded branch was illustrated (white arrow), and the occluded small pulmonary veins were illustrated (green arrows). After three months of dabigatran therapy, an axial image demonstrating F: the thrombus was dissolved. Something appeared to be left (white arrow), which may be the fibrin network of the thrombus. G: a new enhanced small pulmonary vein appeared (green arrows), indicating that dabigatran dissolved the thrombi in the small pulmonary veins. (C, H) H: A new enhanced small pulmonary vein seemed to appear (red arrow), and there seemed to be a collapsed pulmonary vein in panel C that was not clearly illustrated. A branch of LLPV without a thrombus was illustrated in panels E and J (white arrowhead). |
Because 64-MDCT can assess even small arteries accurately, it could be utilized to assess pulmonary vein thrombus. As I reported, some patients with chest pain had pulmonary vein thrombi [3]; [4]; [5]; [6]; [7]; [8]; [9] ; [10]; we can utilize a 64-MDCT scan to decide the optimum duration of DAPT if the patients have pulmonary vein thrombi and DAPT can dissolve pulmonary vein thrombi. Even if DAPT does not dissolve pulmonary vein thrombi, DAPT may be useful if it can inhibit the growth of pulmonary vein thrombi or the production of microclots. Moreover, we can change antithrombotic drugs if DAPT has no ability to dissolve a pulmonary vein thrombus. To choose optimum antithrombotic drugs, 64-MDCT may be useful. More studies are required to use 64-MDCT for this purpose.
It may be possible to decide the optimum duration of DAPT, as assessed by the change of pulmonary vein thrombi using 64-MDCT.
Conflict of interest
The author reports no relationships that could be construed as a conflict of interest.
References
- [1] L. Mauri, D.J. Kereiakes, R.W. Yeh, P. Driscoll-Shempp, D.E. Cutlip, P.G. Steg, et al.; Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents; N Engl J Med, 371 (2014), pp. 2155–2166
- [2] T. Palmerini, U. Benedetto, L. Bacchi-Reggiani, D.D. Riva, G. Biondi-Zoccai, F. Feres, et al.; Mortality in patients treated with extended duration dual antiplatelet therapy after drug-eluting stent implantation: a pairwise and Bayesian network meta-analysis of randomised trials; Lancet (2015 March 13) https://doi.org/10.1016/SS0140-6736(15)60263-X
- [3] H. Takeuchi; A thrombus of the right upper pulmonary vein: detection by the use of a 64-MDCT; BMJ Case Rep (Sep 2012 14) https://doi.org/10.1136/bcr.12.2011.5446 (Published online)
- [4] H. Takeuchi; High prevalence of pulmonary vein thrombi in elderly patients with chest pain, which has relationships with aging associated diseases; IJC Heart & Vessels, 4 (2014), pp. 129–134 https://doi.org/10.1016/j.ijchv.2014.05.006 (Published online: 6-JUN-2014)
- [5] H. Takeuchi; A network of pulmonary vein thrombi is a risk factor for ischemic stroke, especially after cardiac surgery: a case report and mini review; IJC Heart & Vasculature, 6 (2015), pp. 1–3
- [6] H. Takeuchi; Nearly all left atrial thrombi may be extended from pulmonary vein thrombi; IJC Heart & Vasculature, 7 (2015), p. 9
- [7] H. Takeuchi; A long and narrow pulmonary vein thrombus attached to the wall of pulmonary vein; IJC Heart & Vasculature, 7 (2015), pp. 49–50
- [8] H. Takeuchi; Pulmonary vein thrombosis is associated with chest pain in patients without coronary artery stenosis; IJC Heart & Vasculature (2015) https://doi.org/10.1016/j.ijcha.2015.02.009
- [9] H. Takeuchi; 64-slice multidetector computed tomography may assess resistance of antiplatelet drugs; Int J Cardiol (2015) https://doi.org/10.1016/j.ijcme.2015.03.001
- [10] H. Takeuchi; Implementation of 64-MDCT assesses that short-term warfarin therapy can dissolve a completely occluding small thrombus: a new clue to treat atrial fibrillation; IJC Heart & Vasculature, 7 (2015), pp. 146–148
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?