Abstract
Stroke remains a devastating complication following cardiac surgery. Pulmonary vein thrombi (PVT) are believed to be rare, but I have reported 37 cases of PVT in elderly patients with chest pain since 2012, indicating that PVT are not unusual. The present case showed that PVT can make a network among four pulmonary veins and left atrium. Currently, PVT are not recognized as a risk factor for ischemic stroke, especially following cardiac surgery.
A 76-year-old male was examined by 64-slice multidetector CT (64-MDCT) to assess chest pain. The 64-MDCT scan revealed thrombi in the left upper and lower pulmonary veins, the right upper and lower pulmonary veins and the left atrium (LA) as the defects of contrast enhancements. The LA thrombi seemed to be connected to PVT forming a network of thrombi.
To avoid stroke following cardiac surgery, it is important to cope with PVT. How to treat PVT during cardiac surgery should be developed.
Keywords
Ischemic stroke;Cardiac surgery;Pulmonary vein thrombi;Dabigatran;64-MDCT
1. Introduction
Stroke remains a devastating complication following cardiac surgery, which occurs in 3% to 9% of patients after cardiac surgery [1]. Patients with postoperative strokes have up to a 10-fold increase in mortality [2] ; [3].
Pulmonary vein thrombi (PVT) have been reported in cases of primary and secondary tumors of the lung or as a rare complication occurring immediately after thoracic surgical procedures, such as lobectomy, bilobectomy, left thoracoplasty performed 50 years earlier for tuberculosis [4] or lung transplantation. These cases have been diagnosed using transoesophageal echocardiography. PVT have been believed to be rare until recently.
Since 2012, I have reported 37 cases of PVT in elderly patients without such conditions using 64-slice multidetector computed tomography (64-MDCT) [5] ; [6], which suggests that PVT are not rare in elderly patients. Recently, I have reported 61% of the 57 elderly patients with chest pain had PVT [7], which proved PVT are not uncommon. However, there have been no previous reports of PVT network formation. Although I have reported PVT in patient with cerebral infarction [5], PVT are not generally recognized as a risk factor for ischemic stroke, especially following cardiac surgery. During cardiac surgery, this network of PVT will be broken, which may make it easy to cause ischemic stroke more frequently.
In this case report, I show a network of PVT and discuss the effects of cardiac surgery on PVT that may cause ischemic stroke more easily, which is a crucial issue because ischemic stroke after otherwise successful cardiac surgery is a serious concern for patients and their families.
2. Case presentation
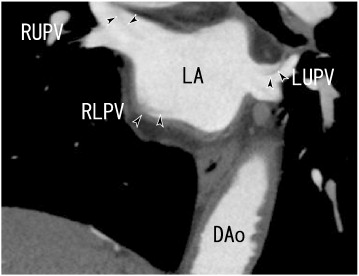
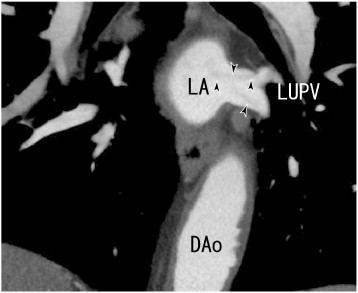
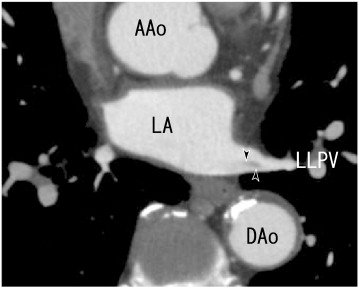
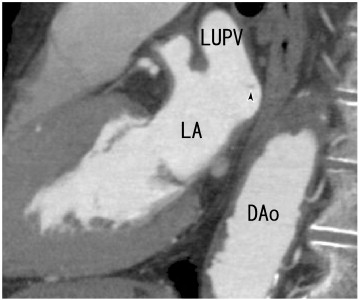
A 76-year-old man experienced chest pain. He had no symptoms of cerebral infarction or lung cancer. The patient had no history of smoking or symptoms of tachypnea, fever, cough, sputum, palpitation or cerebral infarction. The lung examination did not reveal decreased breath sounds, lung crackles or wheezing. The cardiac examination did not demonstrate a heart murmur or arrhythmia. He had no history of recurrent atrial fibrillation or airway infections, and he was not treated with antithrombotic or anti-platelet drugs. The chest roentgenogram did not reveal lung cancer. The serum d-dimer level was < 0.5 μg/mL (normal < 1.0 μg/mL); the protein S activity was 91% (normal 60–150%); and the protein C activity was 66% (normal 64–146%). 64-MDCT was performed to check for coronary artery stenosis, and it revealed thrombi in the left upper and left lower pulmonary veins (LUPV and LLPV), the right upper and lower pulmonary veins (RUPV and RLPV), and the left atrium (LA) as defects of contrast enhancements (Fig. 1, Fig. 2, Fig. 3, Fig. 4 ; Fig. 5). The LA thrombi seemed to be connected to the thrombi of four pulmonary veins, potentially representing a network of thrombi.
|
|
|
Fig. 1. A 64-slice multidetector CT (64-MDCT) scan showed coronal images of thrombi in the right and left upper pulmonary veins (RUPV and LUPV) and in the left atrium (LA), which seemed to be connected to thrombi in the right lower pulmonary vein (RLPV) (arrowheads). DAo: descending aorta, LA: left atrium, LUPV: left upper pulmonary vein, RLPV: right lower pulmonary vein, and RUPV: right upper pulmonary vein. |
|
|
|
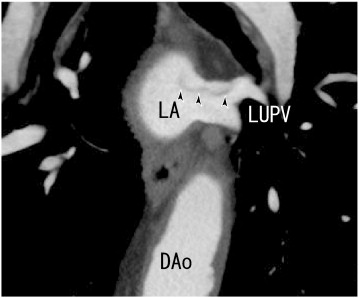
Fig. 2. A 64-MDCT scan showed coronal images of thrombi in the LUPV (arrowheads). DAo: descending aorta, LA: left atrium, and LUPV: left upper pulmonary vein. |
|
|
|
Fig. 3. 64-MDCT axial images showed thrombi in the left lower pulmonary vein (LLPV) (arrowheads). AAo: ascending aorta, DAo: descending aorta, LA: left atrium, and LLPV: left lower pulmonary vein. |
|
|
|
Fig. 4. 64-MDCT sagittal images showed thrombi in the LA (arrowhead). DAo: descending aorta, LA: left atrium, and LUPV: left upper pulmonary vein. |
|
|
|
Fig. 5. 64-MDCT coronal images showed thrombi in the LUPV, illustrated more clearly than those in Fig. 3 (arrowheads). DAo: descending aorta, LA: left atrium, and LUPV: left upper pulmonary vein. |
3. Discussion
This case report demonstrated a network of PVT in a 76-year-old male without atrial fibrillation. He was not treated with antithrombotic or anti-platelet drugs. It is important to know the existence of PVT and to identify PVT using 64-MDCT, which is not rare and can make a network. PVT are not uncommon, but forming a network of PVT may be not so often as assessed using 64-MDCT. A network of PVT will be broken during cardiac surgery, which can cause cerebral infarction more frequently.
Ischemic stroke after cardiac surgery is serious clinical problem [1]. Presently, PVT and a network of PVT are not recognized as a risk factor, which can cause ischemic stroke after cardiac surgery. It is important to develop how to cope with PVT during cardiac surgery.
PVT had root in the small pulmonary vein, which grew into a larger thrombus in the larger pulmonary vein [8]. The fibrin network and the attached thrombin are two main components of a thrombus. Dabigatran is a thrombin inhibitor, which has some preventive effects on thrombin binding ability to the fibrin network and may have indirect effects on the fibrin network by decreasing the number of thrombin attached to the fibrin network. If the fibrin network is small and the blood flow around the thrombus is rich, then it seemed to be dissolved [6]. But if PVT are larger, then some structure was left after the thrombus was incompletely dissolved by dabigatran therapy [7] ; [9]. The remained structure might be mainly the fibrin network.
In PVT, the fibrin network in a thrombus has deep long root in smaller pulmonary vein and the structure of the fibrin network and the thrombus may be stable, so the rate of ischemic stroke decreased. But in thrombi of the patients with the cardiac surgery, the fibrin network will be broken during the cardiac surgery and the thrombi don't have long roots in the pulmonary vein in some cases, so it could cause ischemic stroke more easily during dabigatran therapy.
Although in RE-LY trial, dabigatran decreased the rate of thromboembolic events [10], dabigatran increased the rate of thromboembolic events in RE-ALIGN study [11]. RE-ALIGN study treated the patients with mechanical heart valve. The character of a thrombus in the patients with mechanical heart valve may be different from that of a thrombus in the patients with atrial fibrillation. RE-ALIGN study showed high prevalence of thromboembolism by using dabigatran to compare with warfarin, which may be caused by being broken of PVT or a network of PVT.
There is a clue in my reported case reports. I have reported that warfarin dissolved a thrombus in the pulmonary vein completely [5] and a thrombus in the left atrial appendage partially [12]. Some parts of the thrombus in the left atrial appendage was dissolved, which borderline was clear [12], indicating no structure, no fibrin network, was left. Warfarin seemed to dissolve fibrin network more efficiently with another mechanism.
Pulmonary vein thrombi can release microclots, which can occlude the microvessels of all of the organs, including bones, skeletal muscles, and coronary arteries. Occluded microvessels cannot supply moderate oxygen or nutrients and cannot remove harmful compounds, such as waste products and carbon dioxide, from organs. Such conditions inhibit the normal functions of organs. It is important to study relationships between the fibrin network and pathologic clots that can occlude microvessels in all organs and larger arteries such as cerebral artery and coronary artery and to study the effects of warfarin and dabigatran on them.
4. Conclusion
This case report demonstrated a network of PVT in a 76-year-old male without atrial fibrillation nor antithrombotic or anti-platelet treatment. The LA thrombi might be linked to the thrombi of four pulmonary veins, potentially representing a network of thrombi. PVT can cause thromboembolism such as ischemic stroke, especially after cardiac surgery. How to cope with PVT in cardiac surgery should be developed. The results of both RE-LY trial and RE-ALIGN study are right. It may be important to recognize the existence of a network of PVT, which may be broken during cardiac surgery.
Conflict of interest
The authors report no relationships that could be construed as a conflict of interest.
References
- [1] G.M. McKhann, M.A. Grega, L.M. Borowicz Jr., W.A. Baumgartner, O.A. Selnes; Stroke and encephalopathy after cardiac surgery. An update; Stroke, 37 (2006), pp. 562–571
- [2] G.M. McKhann, M.A. Goldsborough, L.M. Borowicz, E.D. Mellits, R. Brookmeyer, S.A. Quaskey, et al.; Predictors of stroke risk in coronary artery bypass patients; Ann Thorac Surg, 63 (1997), pp. 516–521
- [3] G.W. Roach, M. Kanchuger, C.M. Mangano, M. Newman, N. Nussmeier, R. Wolman, et al.; Adverse cerebral outcomes after coronary bypass surgery; N Engl J Med, 335 (1996), pp. 1857–1863
- [4] M.J. Garcia, L. Rodriguez, P. Vandervoort; Pulmonary vein thrombosis and peripheral embolization; Chest, 109 (1996), pp. 846–847
- [5] H. Takeuchi; A thrombus of the right upper pulmonary vein: detection by the use of a 64-MDCT; BMJ Case Rep (Sep 14 2012) https://doi.org/10.1136/bcr.12.2011.5446 [Published online]
- [6] H. Takeuchi; Floating thrombus in the left upper pulmonary vein dissolved by dabigatran; BMJ Case Rep (Oct 9 2013) https://doi.org/10.1136/bcr-2013-200836 [Published online]
- [7] H. Takeuchi; High prevalence of pulmonary vein thrombi in elderly patients with chest pain, which has relationships with aging associated diseases; IJC Heart Vessels (JUN 6 2014) https://doi.org/10.1016/j.ijchv.2014.05.006 [Published online]
- [8] H. Takeuchi; How to find a thrombus in a small pulmonary vein that is not enhanced by contrast agents because of a lack of arterial blood flow; BMJ Case Rep (Oct 29 2013) https://doi.org/10.1136/bcr-2013-010261 [Published online]
- [9] H. Takeuchi; Chest pain caused by pulmonary vein thrombi could be curable by dabigatran; BMJ Case Rep (March 13 2014) https://doi.org/10.1126/bcr-2013-203186 [Published online]
- [10] S.J. Connolly, M.D. Ezekowitz, S. Yusuf, J. Eikelboom, J. Oldgren, A. Parekh, et al.; Dabigatran versus warfarin in patients with atrial fibrillation; N Engl J Med, 361 (2009), pp. 1139–1151
- [11] J.W. Eikelboom, S.J. Connolly, M. Brueckmann, C.B. Granger, A.P. Kappetein, M.J. Mack, et al.; Dabigatran versus warfarin in patients with mechanical heart valves; N Engl J Med, 369 (2013), pp. 1206–1214
- [12] H. Takeuchi; A 64-slice multi-detector CT scan could evaluate the change of the left atrial appendage thrombi of the atrial fibrillation patient, which was reduced by warfarin therapy; BMJ Case Rep (Aug 19 2011) https://doi.org/10.1136/bcr11.2009.2491 [Published online]
Document information
Published on 19/05/17
Submitted on 19/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?