Abstract
Objectives
The aim of this study was to evaluate the short-term clinical and radiological results of tibiotalocalcaneal arthrodesis (TTCA) with proximal humeral locking plate.
Material and methods
Eight patients (7 female, 1 male; average age 53 years (range: 24–67)) who underwent TTCA with proximal humeral locking plate between 2009 and 2011, were retrospectively evaluated with AOFAS hindfoot scale and Maryland foot score system. The mean follow up was 32.6 months (range: 23–54).
Results
Complete fusion was achieved in 7 patients. Soft tissue infection was observed in 2 patients and reflex sympathetic dystrophy in 3 patients. All patients recovered with medical treatment. At the final follow-up, mean AOFAS Hindfoot score was 60 (range: 41–81) and Maryland Foot Score was 67.8 (range: 41–85). The satisfactory rates of AOFAS and MFS were found as 12.5% (1/8) and 50% (4/8), respectively. One patient had an incomplete union with 5 degrees of heel varus deformity and 5 degrees of equinus deformity was observed in another. There were no implant failure or deformation of the plate during the follow-up period.
Conclusion
Our study suggests that proximal humeral plate may be an alternative for fixation in tibiotalocalcaneal fusion surgery.
Keywords
Tibiotalocalcaneal arthrodesis ; Hindfoot arthrosis ; Proximal humeral locking plate
Introduction
Tibiotalocalcaneal arthrodesis (TTCA) is an effective treatment method in severe arthrosis, deformity, and functional disturbance of degenerated ankle and subtalar joints. Common indications for this procedure include severe arthrosis of ankle and subtalar joints, talus avascular necrosis, Charcot arthropathy, neuromuscular disorders, and failure of ankle arthroplasty.1
Many kinds of fixation methods have been described to achieve adequate tibiotalocalcaneal fusion.2 Stable fixation is mandatory for a good outcome in TTCA. For this purpose, different types of fixation devices—including angled plates, screws, external fixation devices, and in particular, intramedullary nails (IMN)—have been used.3
Major complications of TTCA are nonunion, malunion, infection, and wound complications.4 Proximal humeral locking plates, which biomechanical studies have demonstrated to provide rigid fixation, are gaining popularity as a reliable fixation material capable of achieving stable and adequate alignment.2 ; 5 ; 6 Previous studies have reported that the technical application of proximal humeral locking plates is easier than that of IMN and angled plates.6 ; 7 It has also been demonstrated that locking plates possess superior biomechanical stability; this is especially true in osteopenic and osteoporotic patients, who compose the majority of the population with ankle arthritis.3 ; 8 Locking plate technology plays a key role in rigid and stable fixation.6
The aim of this study was to evaluate short-term outcomes of TTCA procedure using proximal humeral locking plate.
Material and methods
Between 2009 and 2011, 9 patients with tibiotalocalcaneal arthrosis who had undergone TTCA with proximal humeral locking plate were evaluated retrospectively. One patient was excluded from the study because of limited follow-up; thus, 8 patients were included. None of the patients had undergone prior arthrodesis surgery for tibiotalocalcaneal arthrosis. Etiologies of tibiotalocalcaneal arthrosis were primary in 2 patients, secondary to trauma in 1 patient, due to neuropathy in 2 patients, secondary to deformity in 2 patients (1 being clubfoot), and secondary to talus avascular necrosis in 1 patient. All patients were reviewed with anteroposterior and lateral X-ray, and at final follow-up they were assessed with American Orthopaedic Foot and Ankle Society (AOFAS) Hindfoot Score and Maryland Foot Score (MFS). Seven patients were female (87.5%), and 1 patient was male (12.5%). At time of operation, average age was 53 years (range: 24–67 years), and mean duration of postoperative follow-up was 32.6 months (range: 23–54 months). Five of the patients had right side (62.5%), and 3 had left side (37.5%) involvement. According to the American Society of Anesthesiologist (ASA) classification system, 6 of the patients had ASA 1, and 2 of the patients had ASA 2 scores, preoperatively (Table 1 ).
| Patient | Age | Gender | Etiology of arthrosis | Side | Follow-up (months) |
|---|---|---|---|---|---|
| 1 | 66 | Female | Primary | R | 23 |
| 2 | 55 | Female | Clubfoot | R | 31 |
| 3 | 46 | Female | Primary | L | 25 |
| 4 | 56 | Female | Neuropathy | R | 31 |
| 5 | 67 | Female | Avascular necrosis | L | 28 |
| 6 | 63 | Female | Neuropathy | R | 44 |
| 7 | 24 | Male | Deformity | R | 25 |
| 8 | 47 | Female | Trauma | L | 54 |
| Mean | 53 | 32.625 |
All procedures were performed under spinal and epidural combined regional anesthesia by a single orthopedic surgeon. Patients were placed in supine position with ipsilateral gluteal elevation for ease of approach. For the exposure, transfibular approach was used with distal fibula resection. Both tibiotalar and talocalcaneal joint surfaces were trimmed and prepared for arthrodesis. All surgical procedures were performed in the same sequence, with the exception of the patient with talus avascular necrosis. In that case, the talus was excised, and the resected distal fibula, which was divided in half, was used as a double strut graft to maintain the height of the extracted talus. Allograft was not applied during any surgery. The objectives for ankle alignment were to achieve neutral flexion, 0°–5° of valgus, and 5°–10° of external rotation.7 Arthrodesis was stabilized with 114-mm PHILOS Plate (Synthes, Paoli, PA, USA) in 3 patients and with 14-hole Proximal Humeral Locking Plate (TST, Istanbul, Turkey) in 5 patients. Plates were applied by inversion. At least 6 cortices were attached by locking screws on both tibial and calcaneal sides and without additional lag screws. A drain was applied upon completion of surgery and was removed after 24 h.
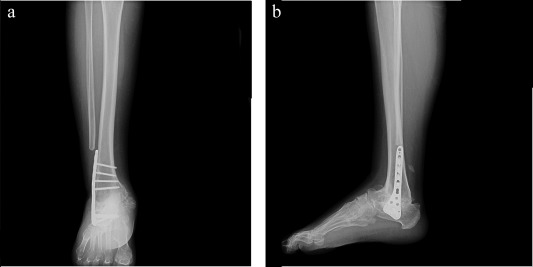
A short leg non-weight-bearing cast was applied postoperatively for 8–12 weeks. After cast removal, gradual weight-bearing was allowed with solid ankle foot orthoses until solid healing was observed. Full weight-bearing was permitted when solid fusion was achieved according to clinical and radiological examination. At 6 weeks, 3 months, 6 months, and 1 year postoperatively, X-rays were obtained to evaluate ankle fusion (Fig. 1 ; Fig. 2 a, b).
|
|
|
Fig. 1. (a–c). Preoperative anteroposterior-lateral and oblique X-ray views of 56-year-old female ankle arthrosis patient. |
|
|
|
Fig. 2. (a and b). Postoperative anteroposterior and lateral views at 6-month follow-up. |
Results
Solid union was achieved in subtalar and tibiotalar joints in 7 patients (87.5%). One patient experienced incomplete union, which caused mild pain during ambulation. Mean union time was evaluated as 17.3 weeks. One patient healed with 5° of mild equinus deformity, in which the etiology was secondary to peripheral neuropathy; in the patient with incomplete union, 5° of mild heel varus deformity was observed. Soft-tissue infection was observed in 2 patients postoperatively, which was treated with oral antibiotics and wound care. Reflex sympathetic dystrophy was observed in 3 patients and was resolved with physical therapy (Table 3 ). At final follow-up, mean AOFAS Hindfoot Score was 60 (range: 41–81), and mean MFS was 67.8 (range: 41–85) (Table 2 ). Satisfaction rates of AOFAS and MFS were 12.5% (1/8) and 50% (4/8), respectively. During the follow-up period, no hardware breakage or deformation was observed, nor did any patients require surgical removal of hardware.
| Patient | AOFAS score | Maryland foot score |
|---|---|---|
| 1 | 70 | 77 |
| 2 | 50 | 65 |
| 3 | 65 | 84 |
| 4 | 41 | 54 |
| 5 | 48 | 57 |
| 6 | 48 | 41 |
| 7 | 77 | 80 |
| 8 | 81 | 85 |
| Mean | 60 | 67.875 |
AOFAS: American Orthopaedic Foot and Ankle Society.
AOFAS Score: Bad: <69; Fair: 70–79; Good: 80–89; Excellent: 90–100.
Maryland Foot Score: Failure: <50; Fair: 50–74; Good: 75–89; Excellent: 90–100.
| Incomplete union and 5° heel varus deformity | 1 patient |
| 5° equinus deformity | 1 patient |
| Soft tissue infection | 2 patients |
| Reflex sympathetic dystrophy | 3 patients |
Discussion
TTCA is a salvage procedure undertaken for hindfoot problems that affect both the ankle and subtalar joints. Fixation can be achieved with screws, external fixators, angled plates, and frequently with IMN. Despite the availability of different fixation devices, no consensus has been reached in terms of which one is preferable.3 Locking plates have been reported in the literature as being a safe and effective fixation device.6
Various studies have investigated the biomechanical stability of TTCA devices. Chiodo et al showed that angled plates and screws can achieve superior biomechanical stability compared to IMN, in particular in osteopenic patients.8 Comparing bending and initial torsional rigidity between IMN and angled plates, Alfahd et al did not find any significant difference.9 Comparing 3 cross screws, IMN, and 2 cross screws, Bennett et al found that 3 cross screws can achieve more stable fixation.10 Chodos et al compared locking plates with angled plates and demonstrated the superiority of fixation with locking plates.5 O'Neill et al compared initial and final dorsiflexion stiffness, deformation, and loading failure ratios between locking plates and IMN and found that except for final stiffness, locking plates had better results than IMN. They also stated that locking plates can be used as an effective device in TTCA.6 In their biomechanical study, Ohlson et al compared augmented screws with IMN and augmented screws with humeral locking plates and found no significant difference between initial and final stiffness, loading, and structural deformation forces.11
In the literature, IMN is frequently chosen as a fixation device for TTCA.12 ; 13 ; 14 In reviewing 613 cases in 33 studies investigating union complication rates of TTCA with IMN, Jehan et al found union rate to be 86.7%, with 55.7% complication and 22% reoperation rates. Arthrodesis revision rate was 3%. Jehan et al indicated that TTCA with IMN has a relatively good union rate but high complication rate. The majority of complications were related to the metalwork.15
In the studies by O'Neill et al and DiDomenico and Wargo-Dorsey—published in 2008 and 2012, respectively—it was stated that femoral locking plate for TTCA is an easier device in terms of technical application than other available alternatives.6 ; 7
In the current literature, the most extensive study for TTCA with locking plate was conducted by Ahmed et al, who chose proximal humeral locking plate not only for the multiplanar internal stability created with the plate between the tibia, talus, and calcaneus but also the congruity of the plate with the regional anatomy. Ahmed et al achieved fusion in 17 of 18 arthrodeses (94.4%), with a final mean AOFAS score of 76.7. They reported that this technique could be effective in osteopenic bone.2
Lowery et al discussed the effectiveness of proximal humeral locking plates in TTCA in a case study of a peripheral neuropathy patient. TTCA was performed with 6.5-mm cannulated compression screws and proximal humeral locking plate. A bone stimulator was implanted to achieve bony fusion. Lowery et al recommended the use of an interfragmentary compression screw in such cases.3
The results of the present study are similar to those of 2 published papers addressing TTCA with proximal humeral plate.2 ; 3 While our union rates (85%) were similar to those in Ahmed et als previous reports, the mean functional score was lower (60; range: 41–81). We believe this finding is related with the co-morbidities of the patients, which affect ambulatory status regardless of the presence or absence of pain. However, TTCA is a non-physiological salvage procedure.
In the current literature, there is no consensus regarding best choice of locking plate type, such as femoral or proximal humerus locking plates, for TTCA fixation. Additionally, the number and type (locked vs non-locked) of the screws used in TTCA vary according to surgeons' preferences.2 ; 3 ; 5 ; 7 However, it has been shown that hybrid fixation (locked plus non-locked screws) is 7% stronger in bending, 42% stronger in torsion, and only 7% weaker in axial strength than all locked fixation types.16 Thus, a hybrid construct can achieve more stable fixation on the diaphysis of the osteoporotic bone.
Previous authors have suggested applying a lag screw passing through the tibiotalar and TTCA sides prior to plate implantation.2 ; 5 In the present study, a lag screw was not used for compression before plate application, though fusion rates have been reported in the literature.2
Second to that of Ahmed et al, ours contains the largest number of subjects in a study on this topic in the literature. Union ratio, AOFAS Hindfoot Score, and MFS results were satisfactory. Our findings demonstrate that use of proximal humeral locking plate for TTCA is an easy method with an acceptable complication rate. No hardware breakage or deformation occurred during the follow-up period.
Limitations of the present study include short duration of follow-up and small number of patients. While 32 months is adequate for the evaluation of fusion procedures, it is insufficient to determine functional measurements. Furthermore, preoperative functional scores are lacking due to the retrospective design of the study.
In conclusion, despite the limited number of patients, the findings of the present study support use of proximal humeral plate for tibiotalocalcaneal fusion.
Conflict of interest
None declared.
References
- 1 B.D.S.C. Blankenhorn; Ankle arthritis; C.S. MJ Coughlin, R.B. Anderson (Eds.), Manns Surgery of the Foot and Ankle, Elsevier (2014), pp. 1037–1077
- 2 J. Ahmad, A.E. Pour, S.M. Raikin; The modified use of a proximal humeral locking plate for tibiotalocalcaneal arthrodesis; Foot Ankle Int, 28 (2007), pp. 977–983
- 3 N.J. Lowery, A.M. Joseph, P.R. Burns; Tibiotalocalcaneal arthrodesis with the use of a humeral locking plate; Clin Podiatr Med Surg, 26 (2009), pp. 485–492 Table of Contents
- 4 P.S. Cooper; Complications of ankle and tibiotalocalcaneal arthrodesis; Clin Orthop Relat Res, 391 (2001), pp. 33–44
- 5 M.D. Chodos, B.G. Parks, L.C. Schon, G.P. Guyton, J.T. Campbell; Blade plate compared with locking plate for tibiotalocalcaneal arthrodesis: a cadaver study; Foot Ankle Int, 29 (2008), pp. 219–224
- 6 P.J. O'Neill, K.J. Logel, B.G. Parks, L.C. Schon; Rigidity comparison of locking plate and intramedullary fixation for tibiotalocalcaneal arthrodesis; Foot Ankle Int, 29 (2008), pp. 581–586
- 7 L.A. DiDomenico, M. Wargo-Dorsey; Tibiotalocalcaneal arthrodesis using a femoral locking plate; J Foot Ankle Surg, 51 (2012), pp. 128–132
- 8 C.P. Chiodo, J.I. Acevedo, V.J. Sammarco, et al.; Intramedullary rod fixation compared with blade-plate-and-screw fixation for tibiotalocalcaneal arthrodesis: a biomechanical investigation; J Bone Jt Surg Am (2003), pp. 2425–2428 85-A(12)
- 9 U. Alfahd, S.E. Roth, D. Stephen, C.M. Whyne; Biomechanical comparison of intramedullary nail and blade plate fixation for tibiotalocalcaneal arthrodesis; J Orthop Trauma, 19 (2005), pp. 703–708
- 10 G.L. Bennett, B. Cameron, G. Njus, M. Saunders, D.B. Kay; Tibiotalocalcaneal arthrodesis: a biomechanical assessment of stability; Foot Ankle Int, 26 (2005), pp. 530–536
- 11 B.L. Ohlson, M.W. Shatby, B.G. Parks, K.L. White, L.C. Schon; Periarticular locking plate vs intramedullary nail for tibiotalocalcaneal arthrodesis: a biomechanical investigation; Am J Orthop (Belle Mead NJ), 40 (2011), pp. 78–83
- 12 T. Muckley, K. Klos, T. Drechsel, C. Beimel, F. Gras, G.O. Hofmann; Short-term outcome of retrograde tibiotalocalcaneal arthrodesis with a curved intramedullary nail; Foot Ankle Int, 32 (2011), pp. 47–56
- 13 T.T. Niinimaki, T.M. Klemola, J.I. Leppilahti; Tibiotalocalcaneal arthrodesis with a compressive retrograde intramedullary nail: a report of 34 consecutive patients; Foot Ankle Int, 28 (2007), pp. 431–434
- 14 R.L. Thomas, V. Sathe, S.I. Habib; The use of intramedullary nails in tibiotalocalcaneal arthrodesis; J Am Acad Orthop Surg, 20 (2012), pp. 1–7
- 15 S. Jehan, M. Shakeel, A.J. Bing, S.O. Hill; The success of tibiotalocalcaneal arthrodesis with intramedullary nailing–a systematic review of the literature; Acta Orthop Belg, 77 (2011), pp. 644–651
- 16 J. Doornink, D.C. Fitzpatrick, S. Boldhaus, S.M. Madey, M. Bottlang; Effects of hybrid plating with locked and nonlocked screws on the strength of locked plating constructs in the osteoporotic diaphysis; J Trauma, 69 (2010), pp. 411–417
Document information
Published on 31/03/17
Licence: Other
Share this document
claim authorship
Are you one of the authors of this document?