Summary
Objectives
Hemiarthroplasty is recommended for treatment of displaced femoral neck fractures in physically compromised elderly patients. The objective of this study was to analyze survivalof patients aged >80 years after the implantation of either an Austin-Moore type prosthesis or a bipolar bearing prosthesis.
Methods
An Austin-Moore or bipolar hemiarthroplasty was implanted into 120 patients aged >80 years. Demographic data were collected. Survival rate at 5 years and factors related to mortality were analyzed.
Results
Sixty-two patients received Austin-Moore hemiarthroplasty, and 58 received bipolar hemiarthroplasty. No significant differences in gender, comorbid conditions, ASA scores, duration of hospitalization, intraoperative blood loss, duration from injury to operation, or postoperative morbidity between the two groups were found. However, patients who received the Austin-Moore hemiarthroplasty were older and had shorter operation time than those who received bipolar hemiarthroplasty. Kaplan-Meier estimates of 5 years survival were 40.0% for patients who received Austin-Moore hemiarthroplasty, and 62.9% for patients who received bipolar hemiarthroplasty. Cox proportional hazard regression analysis of risks factors of death revealed that patients who underwent Austin-Moore hemiarthroplasty were 2.0-fold more likely to die when compared to those who received bipolar hemiarthroplasty.
Conclusions
Elderly patients who receive bipolar hemiarthroplasty may have a more favorable survival outcome when compared to those who receive unipolar hemiarthroplasty.
Keywords
Austin-Moore hemiarthroplasty;bipolar hemiarthroplasty;elderly patients;femoral neck fracture
1. Introduction
The goal of treating displaced femoral neck fractures in less active, elderly patients is the restoration of prefracture ambulatory function with no associated morbidity or need of further operations. Total hip arthroplasty in this subset of elderly patients is impractical due to the magnitude of surgery, the cardiovascular complications associated with cement usage, and the overall dislocation rate.1 Such patients are thus generally treated with either uncemented unipolar or bipolar hemiarthroplasty, an approach that also eliminates risks seen with reduction and internal fixation, including nonunion, malunion, loss of reduction, and osteonecrosis.
The Austin-Moore hemiarthroplasty has been used for over 6 decades, and continues to be the most frequently performed type of arthroplasty for physiologically compromised and dependent elderly patients.1 ; 2 This fixed, unipolar bearing is cost-effective and has a straightforward insertion method, allowing for early mobilization and restoration of functional status, and thus lower short-term morbidity and mortality.3 ; 4 Long-term results, however, are marred by rapid acetabular articular cartilage erosion (which requires conversion to total hip arthroplasty), pain arising from friction of the metallic femoral head against the acetabulum, femoral loosening, and decreased flexion.5; 6 ; 7 These conditions arise from movement or loosening of the prosthesis in the proximal femur, in addition to mechanical shear forces between the prosthesis and the acetabular cartilage.7
The bipolar type of bearing was conceived to provide the theoretical benefit of decreasing motion at the prosthesis-acetabular interface by transferring shear forces to a second ball-and-socket (polyethylene) type articulation. Early studies revealed promising results of low acetabular wear (but not femoral loosening) and functional superiority over the unipolar system. More recent studies, however, have suggested that the bipolar bearing works as a fixed unipolar bearing, despite its modularity, because of the low coefficient of friction at the cartilage-prosthesis junction.8 A fluoroscopic study of movement by Verberne conducted at 1 year postoperatively indicated that many bipolar bearings act as a unipolar implant.8 It is unknown how exactly much bearing motion is required to decrease mechanical stress in vivo.
Comparisons of modern unipolar and bipolar hemiarthroplasties have indicated similar morbidity, mortality, functional outcomes,9; 10; 11; 12; 13 ; 14 and similar rates of dislocation, acetabular erosion, reoperations, and deep wound infection.15 Nevertheless, because of the high mortality rate after sustaining an injury in patients older than 70 years,16 these findings have been limited by short-term follow-up (approximately 2 years) and low statistical power.The present study retrospectively analyzed survivalof patients over 80 years of age after the implantation of either an Austin-Moore type prosthesis or a bipolar bearing prosthesis.
2. Materials and methods
In this retrospective study, data of 120 patients admitted from January 2005 to June2010 were collected. Patients included in the analysis met the following criteria: 1) the patient had received either Austin-Moore or bipolar hemiarthroplasty for femoral neck fracture; 2) the patient was aged >80 years; and 3) the fracture was caused by low-energy trauma. Of the 120 patients included in this study, 62 underwent Austin-Moore hemiarthroplasty and 58 patients underwent bipolar hemiarthroplasty with the U1 Bipolar Hip System (United Orthopedic Corporation, Hsinchu, Taiwan). In the Austin-Moore group there were 37 women (59.7%) and 25 men (40.3%) with a mean ± standard deviation (SD) age of 88.73 ± 4.28 years (range 80–98 years). In the bipolar group, there were 38 women (65.5%) and 20 men (34.5%) with a mean age of 86.83 ± 4.35 years (range 81–98 years).
To assess the severity of comorbid conditions at the time of admission, the American Society of Anesthesiologists (ASA) classification was used.17 The ASA system is composed of 5 classifications: 1) normal, healthy; 2) mild systemic disease; 3) severe systemic disease, but not incapacitating; 4) severe incapacitating systemic condition, constant threat to life; and 5) moribund patient.
The following data were collected to evaluate significant risk factors of mortality: age, gender, bed-confinement, ASA score,17 surgical time, blood loss during surgery, time from injury to operation, hospitalization duration, and the presence of diabetes mellitus, stroke, hypertension, heart disease, and mental disorders. In addition, data regarding daily functioning (activities of daily life, ADL) and the ability to walk with or without assistance were also collected. This study was approved by the Institutional Review Board of National Taiwan University Hospital, and the requirement for patient informed consent was waived due to the retrospective nature of the study.
All patients received a prosthetic replacement (Austin-Moore or U1 Bipolar Hip System) and followed a similar postoperative protocol that consisted of mobilization on postoperative Day 3 with protected weight bearing as soon as it was tolerated. Surgeries were performed using a posterior-lateral approach, and in both procedures the femoral neck was cut and the femoral canal reamed so a snug fit of the stem in the proximal femur was attained.
3. Statistical analysis
Independent two-sample t test was used to compare normally distributed continuous data. Chi-square test/Fishers exact test was used to evaluate categorical variables. The Mann-Whitney U test was used to compare groups when data were not normally distributed. Continuous data were described as mean ± SD or number (%). Nonparametric data were described as median (interquartile range). Survival time was measured from the time of operation to death or the last date of follow-up. The Kaplan-Meier method was used to estimate 5-year mortality rates and the log-rank test was used to determined differences in survival between the 2 groups. A Cox proportional hazard model was used to evaluate significant risk factors of5-year mortality. Statistical analyses were performed with SPSS version 15.0 for Windows (SPSS Inc., Chicago, Illinois, USA). A p-value < 0.05 was considered statistically significant.
4. Results
The patient characteristics are presented in Table 1. There were no significant differences in gender, comorbid conditions, ADL, ability to walk without assistance, requirement of a assist device to walk, ASA scores, duration of hospitalization, intraoperative blood loss, duration from injury to operation, or postoperative morbidity between the 2 groups (all, p ≥ 0.05). However, patients who received the Austin-Moore hemiarthroplasty were older and had shorter operation time (75.81 ± 23.12 min vs. 87.24 ± 21.26 min, p = 0.006) than those who received bipolar hemiarthroplasty.
| Austin-Moore group (n = 62) | Bipolar group (n = 58) | p value | |
|---|---|---|---|
| Age (y)a | 88.73 ± 4.28 | 86.83 ± 4.35 | 0.017* |
| Genderb | |||
| Male | 25 (40.3) | 20 (34.5) | 0.509 |
| Female | 37 (59.7) | 38 (65.5) | |
| Comorbid conditions | |||
| Diabetes mellitusb | 19 (30.6) | 18 (31.0) | 0.963 |
| CVAb | 14 (22.6) | 8 (13.8) | 0.214 |
| Hypertensionb | 33 (53.2) | 36 (62.1) | 0.327 |
| Heart diseaseb | 22 (35.5) | 13 (22.4) | 0.115 |
| Mental diseaseb | 10 (16.1) | 14 (24.1) | 0.273 |
| Bedriddenb | 6 (9.7) | 6 (10.3) | 0.903 |
| ADLa | 63.63 ± 11.88 | 66.48 ± 15.83 | 0.271 |
| Walk without assistanceb | 57 (91.9) | 49 (84.5) | 0.204 |
| Walk with assist deviceb | 47 (75.8) | 35 (60.3) | 0.069 |
| Postoperative morbidity | |||
| Infectionb | 8 (12.9) | 6 (10.3) | 0.663 |
| Dislocation b | 9 (14.5) | 4 (6.9) | 0.180 |
| Chronic pain c | 3 (4.8) | 3 (5.2) | 1.000 |
| ASA scored | |||
| 1 | 2 (3.2) | 1 (1.7) | 0.410 |
| 2 | 21 (33.9) | 25 (43.1) | |
| 3 | 37 (59.7) | 31 (35.4) | |
| 4 | 2 (3.2) | 1 (1.7) | |
| Operation time (min)a | 75.81 ± 23.12 | 87.24 ± 21.26 | 0.006* |
| Duration of hospitalization (d)a | 9.39 ± 3.02 | 10.05 ± 2.78 | 0.213 |
| Blood loss (mL)d | 150 (100, 250) | 175 (100, 200) | 0.865 |
| Injury to operation time (min)d | 705 (310, 1124) | 685 (250, 1020) | 0.488 |
Data are presented a mean ± standard deviation or as number with interquartile range or percentage in parentheses. ∗Indicates significant difference between groups, p < 0.05. The p-values are base on aindependent two-samples t test, bChi-square test, cFishers exact test, and dMann-Whitney U test.
ADL = activities of daily life; ASA = American Society of Anesthesiologists; CVA = cerebrovascular accident.
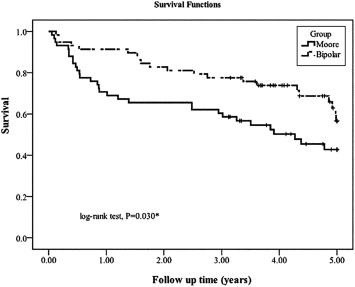
During the follow-up period, 61 patients died; moreover, 35 patients (29.2%) died in the Austin-Moore group and 21 (17.5%) died in the bipolar group within 5 years. As shown in Fig. 1, the Kaplan-Meier estimates of the 5-year survival rates were 62.9 ± 7.1% for patients who received bipolar hemiarthroplasty and 40.0 ± 6.7% for the patients who received the Austin-Moore hemiarthroplasty. The log-rank test revealed a statistically significant difference between the survival rates over time (p = 0.010).
|
|
|
Figure 1. Kaplan-Meier survival curves of patients over 80 years of age after Austin-Moore or bipolar hemiarthroplasty. * Indicates significant difference between groups. |
Results of the Cox proportional hazard regression analysis are presented in Table 2. Age and implant type were identified as significant risk factors of 5-year mortality (p < 0.05). Patients who received the Austin-Moore implant were 2.006 times more likely to die than those who received bipolar hemiarthroplasty (95% confidence interval [CI] 1.167-3.451, p = 0.012).
| HR (95% CI) | p value | |
|---|---|---|
| Age (y) | 1.124 (1.060, 1.193) | 0.001* |
| Gender | ||
| Male | Reference | 0.562 |
| Female | 0.854 (0.501, 1.456) | |
| Comorbid conditiona | ||
| Diabetes mellitus | 1.130 (0.639, 1.998) | 0.674 |
| CVA | 1.211 (0.651, 2.252) | 0.546 |
| Hypertension | 0.995(0.584, 1.695) | 0.986 |
| Heart disease | 0.891 (0.493, 1.610) | 0.701 |
| Mental disease | 0.814 (0.404, 1.682) | 0.596 |
| Bedridden | 0.821 (0.327, 2.058) | 0.674 |
| Implant | ||
| Bipolar | Reference | |
| Austin-Moore | 2.006 (1.167, 3.451) | 0.012* |
| ASA score | 1.419 (0.895, 2.251) | 0.137 |
| Operation time (min) | 0.994 (0.982, 1.006) | 0.314 |
| Duration of hospitalization (d) | 0.943 (0.850, 1.046) | 0.265 |
| Blood loss (mL) | 0.997 (0.994, 1.000) | 0.056 |
| Injury to operation time (min) | 1.000 (0.999, 1.000) | 0.442 |
Results are presented as hazard ratio with 95% confidence interval in parentheses. *Significant risk factor of mortality, p < 0.05. aReference group, yes.
ASA = American Society of Anesthesiologists; CI = confidence interval; CVA = cerebrovascular accident; OR = odds ratio.
5. Discussion
Fractures of the femoral neck have been described as the “beginning of the end for an elderly person”18because of the high 1 year postoperative mortality (19–41%).16 For this reason, early patient mobilization and the avoidance of a second surgery should be a priority in treating displaced femoral neck fractures in the elderly. Our comparison of 62 cases of Austin-Moore hemiarthroplasty and 58 cases of bipolar hemiarthroplasty revealed an estimated 5-year survival rate of 40.0% for the Austin-Moore group and a 62.9% survival rate for the bipolar group, and the difference was statistically significant. Patients who received an Austin-Moore implant were approximately 2 times more likely to die than those who received a bipolar bearing. The reason for better outcomes in the bipolar group may be related to the ball-in-shell mechanism of the bipolar prosthesis, which allows lower acetabular pressure postoperatively than is present with Austin-Moore hemiarthroplasty. The lower acetabular pressure can result in a faster return of the ability to walk, leading to quicker recovery and thus fewer postoperative complications related to immobility.
Studies on long-term patient survival for both unipolar and bipolar hemiarthroplasties are few. Most studies have examined short-term mortality rates, and comparative studies have been largely focused on short-term functional outcomes, quality of life, and complication/reoperation rates.9; 10; 11; 12; 13 ; 14 A study by Pongkunakorn et al19examining cemented hemiarthroplasty in patients with a mean age of 76 years reported a mortality rate at 36 months of 20.8% in those who received unipolar devices and 8.3% in those who received bipolar devices.
Our survival data are consistent with studies which have examined unipolar and bipolar hemiarthroplasties separately. Wachtl et al,20 in a long-term follow-up study of 162 unipolar hemiarthroplasties in women aged >70 years (mean age 84 years) found a survival rate of 73% at 1 year and 23% at 5 years. Patients were treated either by the standard posterior approach or the anterolateral approach according to the surgeons preference. More recently, Norrish et al21 reported a 4-year survival rate of 41% in 500 consecutive patients (mean age, 82 years) treated with Austin-Moore hemiarthroplasty via either a posterior approach or an anterolateral approach.
Long-term patient survival for bipolar hemiarthroplasty has been examined by the Mayo Clinic22 in a study of 224 consecutive patients with a mean age of 79 years. The authors reported mortality rates of 12.3% at 1 year, 20.9% at 2 years, and 44.4% at 5 years. These results are comparable to ours, although our 5-year morality rate was 17.5%. The difference in outcomes may be attributed to the use of cemented femoral fixation in the Mayo Clinic study. Use of cement fixation was not used in our study due the greater risks of embolization and hypotension, and the high proportion of patients with cardiovascular comorbidities (>50%). However, in all cases in our study the stem was carefully fit to the cortex and patients used a walker for assistance for the first 3 postoperative months.
Six large prospective studies9; 10; 11; 12; 13 ; 14 and one Cochrane Review15 have compared the outcomes of unipolar and bipolar hemiarthroplasty. Calder et al9 examined 250 patients aged >80 years who received a Thompson unipolar prosthesis or a Monk bipolar prosthesis. The authors reported survival rates of 75% (unipolar) and 78% (bipolar) at 6 months, and 72% (unipolar) and 69% (bipolar) at 12 months (no statistically significance differences). Davidson et al11 examined cemented unipolar Thompson prostheses and Monk bipolar prostheses in 187 patients aged between 65 and 79 years (median 75 years). The authors reported survival rates of 93% (unipolar) and 90% (bipolar) at 6 months, 89% (unipolar) and 88% (bipolar) at 12 months, and 72% (unipolar) and 78% (bipolar) at 36 months; again, no significant differences were observed. All studies demonstratedthat there are no differences in functional outcome, acetabular erosion, blood loss, reoperation rate, mortality, or infection between unipolar and bipolar hemiarthroplasty.Studies have also found a consistently higher cost for bipolar arthroplasty, ranging from US$700 to US$3,514.15 Similar results were also observed in the present study.
There are limitations to this study that should be considered. First, this was a retrospective analysis of medical records. Different results may be obtained in a prospective, randomized controlled investigation. Thus, it is possible that patients who received bipolar hemiarthroplasty could be in a higher socioeconomic class. Regretfully, we cannot provide data regarding the socioeconomic characteristics of the 2 groups. However, our data indicated that the patients in the 2 groups were similar with respect to their ability to function in daily life as well as ASA scores, suggesting that the 2 groups were in comparable health. Thus, we believe that any influence of socioeconomic class is likely to be small or not present. It can be argued that patients in a higher socioeconomic class may have had access to better postoperative care at home; however, we do not believe it is likely that this would have affected the results.
In summary, the results of the present study suggest that elderly patients who receive bipolar hemiarthroplasty may have more favorable survival when compared to those who receive unipolar hemiarthroplasty. Our findings suggest that further studies with larger samples may be needed to establish definite conclusions as to the optimal surgical treatment for less active elderly patients who sustain femoral neck fractures.
Funding
None.
Acknowledgments
None.
References
- 1 J.S. Gebhard, H.C. Amstutz, D.M. Zinar, F.J. Dorey; A comparison of total hip arthroplasty and hemiarthroplasty for treatment of acute fracture of the femoral neck; Clin Orthop Relat Res, 282 (1992), pp. 123–131
- 2 P.T. Crossman, R.J. Khan, A. MacDowell, A.C. Gardner, N.S. Reddy, G.S. Keene; A survey of the treatment of displaced intracapsular femoral neck fractures in the UK; Injury, 33 (2002), pp. 383–386
- 3 D.C. Kwok, R.L. Cruess; A retrospective study of Moore and Thompson hemiarthroplasty.A review of 599 surgical cases and an analysis of the technical complications; Clin Orthop Relat Res, 169 (1982), pp. 179–185
- 4 R.F. Kyle, M.E. Cabanela, T.A. Russell, et al.; Fractures of the proximal part of the femur; Instr Course Lect, 44 (1995), pp. 227–253
- 5 S.D. Cook, K.A. Thomas, M.A. Kester; Wear characteristics of the canine acetabulum against different femoral prostheses; J Bone Joint Surg Br, 71 (1989), pp. 189–197
- 6 M.B. Gingras, J. Clarke, C.M. Evarts; Prosthetic replacement in femoral neck fractures; Clin Orthop Relat Res, 152 (1980), pp. 147–157
- 7 T.W. Phillips; Thompson hemiarthroplasty and acetabular erosion; J Bone Joint Surg Am, 71 (1989), pp. 913–917
- 8 G.H. Verberne; A femoral head prosthesis with a built-in joint. A radiological study of the movements of the two components; J Bone Joint Surg Br, 65 (1983), pp. 544–547
- 9 S.J. Calder, G.H. Anderson, C. Jagger, W.M. Harper, P.J. Gregg; Unipolaror bipolar prosthesis for displaced intracapsular hip fracture in octogenarians:a randomized prospective study; J Bone Joint Surg Br, 78 (1996), pp. 391–394
- 10 C.N. Cornell, D. Levine, J. O'Doherty, J. Lyden; Unipolar versus bipolar hemiarthroplasty for the treatment of femoral neck fractures in the elderly; Clin Orthop Relat Res, 348 (1998), pp. 67–71
- 11 J.N. Davison, S.J. Calder, G.H. Anderson, et al.; Treatment for displaced intracapsular fracture of the proximal femur.A prospective, randomised trial in patients aged 65 to 79 years; J Bone Joint Surg Br, 83 (2001), pp. 206–212
- 12 R. Malhotra, R. Arya, S. Bhan; Bipolar hemiarthroplasty in femoral neck fractures; Arch Orthop Trauma Surg, 114 (1995), pp. 79–82
- 13 F.J. Raia, C.B. Chapman, M.F. Herrera, M.W. Schweppe, C.B. Michelsen, M.P. Rosenwasser; Unipolar or bipolar hemiarthroplasty for femoral neck fractures in the elderly ?; Clin Orthop Relat Res, 414 (2003), pp. 259–265
- 14 L.L. Rosen, B.J. Miller, P.R. Dupuis, P. Jarzem, A. Hadjipavlou; A prospective randomized study comparing bipolar hip arthroplasty and hemiarthroplasty in elderly patients with subcapital fractures; J Bone Joint Surg Br, 74 (1992), p. 282 [abstract]
- 15 M.J. Parker, K. Gurusamy; Arthroplasties (with and without bone cement) for proximal femoral fractures in adults; Cochrane Database Syst Rev, 2 (2004) CD001706
- 16 L.T. Nilsson, B. Strömqvist, K.G. Thorngren; Nailing of femoral neck fracture. Clinical and sociologic 5-year follow-up of 510 consecutive hips; Acta Orthop Scand, 59 (1988), pp. 365–371
- 17 B.L. White, W.D. Fisher, C.A. Laurin; Rate of mortality for elderly patients after fracture of the hip in the 1980s; J Bone Joint Surg Am, 69 (1987), pp. 1335–1340
- 18 J.T. Johnson, O. Crothers; Nailing versus prosthesis for femoral-neck fractures. A critical review of long-term results in two hundred and thirty-nine consecutive private patients; J Bone Joint Surg Am, 57 (1975), pp. 686–692
- 19 A. Pongkunakorn, P. Thisayukta, P. Palawong; Invention technique and clinical results of Lampang cement injection gun used in hip hemiarthroplasty; J Med Assoc Thai, 92 (Suppl) (2009), pp. S232–S238 6
- 20 S.W. Wachtl, R.P. Jakob, E. Gautier; Ten-year patient and prosthesis survival after unipolar hip hemiarthroplasty in female patients over 70 years old; J Arthroplasty, 18 (2003), pp. 587–591
- 21 A.R. Norrish, J. Rao, M.J. Parker; Prosthesis survivorship and clinical outcome of the Austin Moore hemiarthroplasty: an 8-year mean follow-up of a consecutive series of 500 patients; Injury, 37 (2006), pp. 734–739
- 22 G.J. Haidukewych, T.A. Israel, D.J. Berry; Long-term survivorship of cemented bipolar hemiarthroplasty for fracture of the femoral neck; Clin Orthop Relat Res, 403 (2002), pp. 118–126
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?