(Created page with "==Summary== ====Background==== Anal fissure is a common benign condition. An anorectal problem is defined as a split in the anal canal mucosa that extends from the dentate l...") |
m (Scipediacontent moved page Draft Content 283108404 to Aslam et al 2013a) |
(No difference)
| |
Latest revision as of 11:21, 26 May 2017
Summary
Background
Anal fissure is a common benign condition. An anorectal problem is defined as a split in the anal canal mucosa that extends from the dentate line to the anal verge. Chronic anal fissure is defined by a history of symptoms present for more than 2 months' duration and with a triad of external skin tags, namely, a hypertrophied anal papilla, an ulcer with rolled edges, and a base exposing the internal sphincter. Because complications such as incontinence are associated with surgical treatment, chemical sphincterotomy is currently favored.
Objectives
The objective of this study is to compare the difference in outcome between open partial lateral anal sphincterotomy and application of topical 0.2% nitroglycerin ointment for the treatment of chronic anal fissure.
Methods
This was a quasi-experimental study carried out between January 16, 2007 and January 15, 2008 in the Surgical Department of Jinnah Hospital, Lahore, Pakistan. Sixty consecutive cases with a clinical diagnosis of chronic anal fissure were recruited in the study. All recruited patients met the study inclusion criteria and were randomly assigned to one of the two groups. Group A was managed conservatively using topical 0.2% nitroglycerin ointment, whereas Group B underwent open partial lateral anal sphincterotomy. Both groups were followed up at 1 week, 2 weeks, 4 weeks, and 6 weeks after the treatment.
Results
All the patients complained of pain. A total of 43 (71.7%) patients had pain with constipation, whereas 31 (51.7%) patients had bleeding per rectum. Upon clinically examining the anal area, tenderness was elicited in all 60 (100%) patients. Group A included 30 (11 females and 19 males) cases treated with topical 0.2% nitroglycerin ointment and Group B included 30 (11 females and 19 males) cases who underwent open partial lateral anal sphincterotomy.
In Group A, only 15 patients with fissures were successfully treated (50%). By contrast, 28 (93%) patients with fissures in Group B were successfully treated, and only two (7%) remained uncured. These two patients (6.6%) in Group B suffered from incontinence due to flatus and feces as a complication of the procedure.
Conclusion
This quasi-experimental study demonstrates that open partial lateral internal sphincterotomy is superior to topical 0.2% nitroglycerin application in the treatment of chronic anal fissure, with good symptomatic relief, high rate of healing, fewer side effects, and a very low rate of early continence disturbances.
Keywords
chronic anal fissure;open partial lateral anal sphincterotomy;topical 0.2% nitroglycerin
1. Introduction
Anal fissure is one of the most common lesions to be considered in the differential diagnosis of anal pain. It typically causes episodic pain that occurs during defecation and persists for 1–2 hours afterward.1
The most consistent finding in typical fissures is spasm of the internal anal sphincter, which is so severe that the pain caused by the fissure is thought to be due to ischemia of the sphincter.2 Morbidity from operative procedures, mainly incontinence, was once thought to be extremely rare,3 but has been substantial in some recent reports.4
The choice of treatment remains difficult for the following reasons. Although surgery is highly efficacious and successful in treating the fissure in more than 90% of patients, in a systematic review of randomized surgical trials, the overall risk of incontinence was approximately 10%.5 This was mostly due to flatus incontinence, and there are no reports delineating the duration of this problem.
Regarding medical treatment, in a similar systematic review combining all analyses in which a placebo was used as the comparison group,6 the healing rate in the placebo group was found to be 35%. This was a level of response that was fairly uniform across studies (standard deviation: 12%). The medications being tested in the meta-analysis (nitroglycerin ointment, botulinum toxin injection, and calcium channel blockers) must have their efficacy viewed in the context of this placebo effect and also in the context of a cure rate for surgery that often exceeds 95%.5 In the combined analyses, nitroglycerin ointment was found to have a healing rate of about 55%. In addition, with nitroglycerin ointment, the most investigated medical treatment, headache was common, occurring in almost 40% of patients in the combined analyses and often severe enough to stop treatment.6
Therefore, it would be advantageous if the risk of incontinence could be reduced after the surgery or if the success rate of various other medical treatments is increased to that reported after a surgery, but with less risk of headache.
The risk of using such treatments is not high, as patients mainly only experience headache while using the nitroglycerin ointment, without any apparent adverse effect in the long term. Medical treatments can therefore be used in individuals wanting to avoid surgical treatment, and surgery can be reserved for treatment failures in adults with chronic typical fissure. We wanted to study scientifically whether the outcome of surgical management among these patients is better than conservative (medical) approach.
2. Patients and methods
This was a quasi-experimental study carried out between January 16, 2007 and January 15, 2008 in the Surgical Department of Jinnah Hospital, Lahore, Pakistan (study duration: 1 year). A total of 60 consecutive cases with clinical diagnosis of chronic anal fissure were recruited. All the participants fulfilled the inclusion criteria, which were evaluated using convenient nonprobability sampling.
2.1. Sample size
The 60 patients with chronic anal fissure were divided into two groups, namely, Group A [i.e., topical application of 0.2% nitroglycerin ointment (n = 30 cases)] and Group B [i.e., open partial lateral internal sphincterotomy (n = 30 cases)].
2.2. Inclusion criteria
The study included patients with chronic anal fissure, either gender, and age between 20 years and 60 years.
2.3. Exclusion criteria
The exclusion criteria for the study were as follows: pregnant ladies, patients with inflammatory bowel disease, patients with recurrent anal fissure, patients with hemorrhoids, and those not willing for treatment.
2.4. Ethical issues
All the patients were examined and investigated only after obtaining informed consent. Adequate privacy and presence of chaperone were ensured. Those patients who were treated surgically signed a written consent form.
2.5. Data collection procedure
Sixty consecutive cases of anal fissure diagnosed clinically with digital examination were registered to participate in the study. A written informed consent was obtained from all the patients after they were briefed about the procedures of fissure management. All patients met the inclusion criteria and were randomly assigned to one of the two groups. The demographic data including name, age, gender, and address were recorded. A topical anesthetic ointment (lignocaine gel) was routinely applied 5–10 minutes prior to the patients undergoing digital examination. The patients who were managed conservatively (Group A) were supplied with 0.2% nitroglycerin ointment, and were advised to rub the paste every 8 hours with a gloved finger. The treatment was carried out for 6 weeks. Patients were followed up at 1 week, 2 weeks, 4 weeks, and 6 weeks after the treatment with special consideration to pain relief, healing of fissure, and side effects of treatment. The pain severity was recorded as mild, moderate, and severe. Analgesics, sitz bath, and laxatives were standard options to treat pain. The patient is considered to be successfully healed when the breach in mucosa was completely treated and the patient had not experienced pain during defecation. Group B underwent open partial lateral anal sphincterotomy and the patients were followed up at 1 week, 2 weeks, 4 weeks, and 6 weeks after the treatment.
2.6. Data analysis
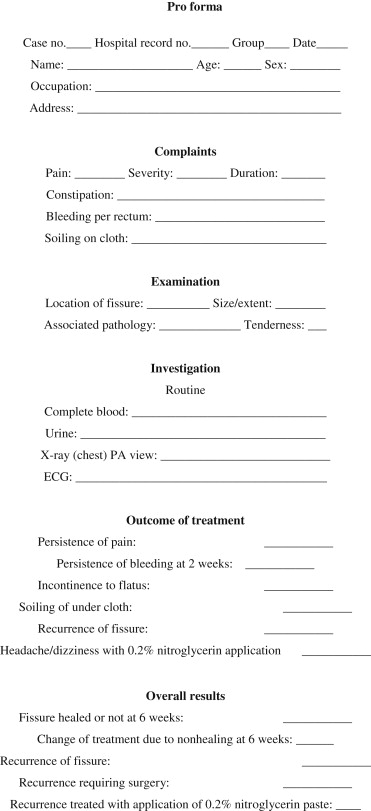
All the information collected was entered in a designed pro forma, as shown in Appendix 1, which was then entered in SPSS (version 10; SPSS Inc, Chicago, IL, USA) and analyzed. The variables analyzed were demographic variables (name, age, gender), severity of pain, constipation, and bleeding per rectum. Quantitative data such as age were presented as mean and standard deviation, whereas qualitative data such as gender and pain were presented as frequency distribution table. A comparison of the outcomes between the two procedures was made by Chi-square test, as the variables were qualitative in nature. A p value <0.05 was considered significant.
3. Results
A total of 60 patients with clinical diagnosis of chronic anal fissure were included in this study. In Group A, the minimum age of the participants was 20 years and the maximum age was 58 years (mean age: 38.20 ± 12.3 years). In Group B, the minimum age of the participants was 21 years and the maximum age of the participants was 58 years (mean age: 38.4 ± 13.03 years). A total of 22 (36.6%) participants were female (11 in each group) and 38 (63.3%) were male (19 in each group).
All the 60 patients complained of pain (100%). However, the severity of pain varied. A total of 13 patients recorded pain as moderate (21.7%), whereas 47 (78.3%) patients recorded it as severe. Constipation was found in 43 (71.7%) cases and 31 (51.7%) individuals presented with bleeding per rectum.
Taking the site of the fissure into account, 49 (81.6%) patients presented with posterior anal fissure, whereas 11 patients (18.4%) presented with anterior anal fissure. Most patients with anterior anal fissure were females. Upon clinically examining the anal area, tenderness was elicited in all the 60 (100%) patients.
No pain was experienced by 17 patients after topical 0.2% nitroglycerin application, but one patient reported persistent pain after lateral internal sphincterotomy.
The bleeding was taken into account at 2 weeks' interval after the completion of treatment. In Group A, which included patients treated with 0.2% nitroglycerin, 17 patients presented with bleeding at 2 weeks' follow-up. By contrast, in Group B, which included patients treated with lateral anal sphincterotomy, only two (6%) patients presented with bleeding at 2 weeks' follow-up.
No headache was reported by 10 (33%) patients in Group A during the treatment with topical 0.2% nitroglycerin. No incontinence was reported by patients in both Group A and Group B; however, two (6.6%) patients developed incontinence due to flatus and feces as a complication of procedure.
In Group A, the anal fissure successfully healed in 15 (50%) patients, whereas in Group B, the anal fissure successfully healed in 28 (93%) patients after lateral anal sphincterotomy (Table 1).
| 0.2% nitroglycerin (n = 30) | Open lateral internal sphincterotomy (n = 30) | p | |
|---|---|---|---|
| No pain after the treatment | 17 | 29 | 0.0001 |
| No bleeding after the treatment | 17 | 28 | 0.001 |
| No headache with the treatment | 10 | 30 | 0.0001 |
| No incontinence after the treatment | 30 | 28 | >0.5 |
| Fissures healed after 6 weeks | 15 | 28 | 0.0001 |
All the patients were followed up until 6 weeks after the completion of treatment and 15 (50%) patients in Group A were not completely cured from the fissure, which reflects the failure of treatment using topical 0.2% nitroglycerin. In Group B, however, 28 (93%) patients were completely cured at 6 weeks' follow-up, which proves the success of lateral anal sphincterotomy as a treatment of choice for anal fissures.
4. Discussion
Historically, the most common approach for relieving the pain associated with spasm of chronic adult anal fissure is surgical, yet no placebo-controlled surgical trials have been carried out. Surgery is usually associated with high costs, increased recovery time, and risk of incontinence. Therefore, by the late 1990s when alternatives to surgery were sought rather than turning back to older treatments, such as lubricants and numbing agents, newer medications were investigated—in each case, a medication that was known to relax muscle spasm was used. Such medications included nitroglycerin ointment, injection of botulinum toxin, and calcium channel blockers, which are either given as tablets or applied topically.
The encouraging results of early clinical trials of 0.2% nitroglycerin suggested that it might find a role in the treatment of anal fissures. Most studies tried to establish the role of 0.2% nitroglycerin as an exogenous nitric oxide providing agent, which is an important neurotransmitter mediating internal anal sphincter relaxant. In these previous studies, anal manometry and assessment of squeeze pressure were the methods used to evaluate the effectiveness of 0.2% nitroglycerin. Manometry showed 2% reduction in maximum resting pressure and squeeze pressure fell by 11%. This is parallel to criteria used in this study, wherein place of objective evidence and improvement in pain and healing of fissure were used to assess treatment efficacy.
Gorfine7 adopted a similar methodology in 1995 that used clinical evidence to assess the efficiency of treatment. A visual analog scale for pain adopted from a previous study proved to be effective yet simple to evaluate the subjective improvement.8
It was seen that the pain score fell more progressively and permanently from 10 to 2 with surgery as compared with 10 to 4 for topical ointment, but after 6 weeks, the score again rose to 6 or 7 in patients treated with topical ointment. Prior to widely adopting this form of treatment, a comparison with the current standard open lateral internal sphincterotomy must be made.
In this study, using a 0.5 mL dose of 0.2% nitroglycerin, we have observed healing of the fissure in 50% of patients after 6 weeks, which is comparable with the results of Lund and Scholefield9 and other studies.2; 7 ; 10 Although 0.2% nitroglycerin was less effective in healing the fissures, it was quite effective in reducing the symptoms and minimizing the pain when used. Once 0.2% nitroglycerin was discontinued, pain recurred in a few patients, following which almost 30% of patients required surgery in this group after 6 weeks.
The fissure healing rate with open partial lateral internal anal sphincterotomy was 93.3%, whereas that for 0.2% nitroglycerin was 50% (p = 0.0001), which is comparable to previous studies, in which the healing rate with open partial lateral anal sphincterotomy was reported to be 94–100%. 11; 12 ; 13
Richard et al14 concluded that surgical sphincterotomy improved healing rate at 6 weeks (89% vs. 29%) and reduced the further requirement for surgery (3% vs. 89%) in his trial of 82 patients.
With regard to symptoms, pain persisted in 13 (43%) patients treated with 0.2% nitroglycerin, whereas only one patient (3.3%) treated surgically complained of persistent pain. Similarly, bleeding per rectum persisted in 13 patients (42%) who applied nitroglycerin ointment. By contrast, bleeding per rectum persisted in only two patients (6%) among those treated surgically.
Incontinence as a complication of the procedure was reported in only two (6.6%) patients treated surgically, which is a result similar to that reported in previous studies.15 ; 16 One might argue that a more objective measure such as anal manometry should have been performed to asses anal sphincter status; however, we felt that the clinical symptom status was more relevant. Although this study suggests that continence is not adversely affected in the short term, further prospective evaluation with a comparison of control groups is needed to determine the long-term effect.
Different studies showed high rate of headache with 0.2% nitroglycerin, but in our study it was 67%, which was controlled by simple analgesics.15 ; 16 A mean healing period of 4 weeks was observed in Group B, whereas for Group A it was 6 weeks, which was similar to that achieved by Coher A,11 Gorfine,7 and Lund and Scholefield.9
A limitation to this study is that patient follow-up was done only for the first 6 weeks after the treatment, which was not enough to reflect any long-term results or recurrence of the symptoms.
In conclusion, this quasi-experimental study demonstrates that open lateral internal anal sphincterotomy is superior to the topical application of 0.2% nitroglycerin ointment in the treatment of anal fissure, with the advantages of good symptomatic relief, high rate of healing, fewer side effects, and a very low rate of early continence disturbances.
Appendix 1.
References
- 1 L.N. Richard; Medical treatments are only marginally better than placebo, but surgery may cause incontinence; BMJ, 327 (2003), pp. 354–355
- 2 W.R. Schouten, J.W. Briel, J.J. Auwerda; Relationship between anal pressure and anodermal blood flow. The vascular pathogenesis of anal fissures; Dis Colon Rectum, 37 (1994), pp. 664–669
- 3 H. Abcarian; Surgical correction of chronic anal fissure: results of lateral internal sphincterotomy vs. fissurectomy—midline sphincterotomy; Dis Colon Rectum, 23 (1980), pp. 31–36
- 4 J. Garcia-Aguilar, C. Belmonte, W.D. Wong, A.C. Lowry, R.D. Madoff; Open vs. closed sphincterotomy for chronic anal fissure: long-term results; Dis Colon Rectum, 39 (1996), pp. 440–443
- 5 R. Nelson; Non surgical therapy for anal fissure; Cochrane Database Syst Rev (4) (2006), p. CD003431
- 6 R. Nelson; Non surgical therapy for anal fissure (protocol for a Cochrane review); Cochrane Library (2003)
- 7 S.R. Gorfine; Topical nitroglycerin therapy for anal fissures and ulcers; N Engl J Med, 333 (1995), pp. 1156–1157
- 8 M. Salim; History of pain relief and pain measurement; M. Salim (Ed.), Clinical Management of Pain (1st ed.), The Army Press, Rawalpindi, Pakistan (1994), pp. 1–24
- 9 J.N. Lund, J.H. Scholefield; Aetiology and treatment of anal fissure; Br J Surg, 83 (1996), pp. 1335–1344
- 10 R. Rajasundaram, R. Ayyathurai, S. Narayanan, A. Maw; Botulinum toxin A and chronic anal fissures—a literature review; J Eur Surg, 38 (2006), pp. 353–358
- 11 A. Cohen, T.C. Dehn; Lateral subcutaneous sphincterotomy for treatment of anal fissure in children; Br J Surg, 82 (1995), pp. 1341–1342
- 12 T.H. Lewis, M.L. Corman, E.D. Prager, W.G. Robertson; Long-term results of open and closed sphincterotomy for anal fissure; Dis Colon Rectum, 31 (1988), pp. 368–371
- 13 R.V. Bailey, R.J. Rubin, E.P. Salvati; Lateral internal sphincterotomy; Dis Colon Rectum, 21 (1978), pp. 584–586
- 14 C.S. Richard, R. Gregoire, E.A. Plewes, et al.; Internal sphincterotomy is superior to topical nitroglycerin in the treatment of chronic anal fissure: results of a randomized, controlled trial by the Canadian Colorectal Surgical Trials Group; Dis Colon Rectum, 43 (2000), pp. 1048–1057
- 15 A. Farooq, Z. Niaz; Comparative study of lateral internal sphincterotomy versus topical glyceryl trinitrate for treatment of fissure in ano; Ann KEMC, 9 (2003), pp. 278–281
- 16 B.F. Zuberi, Q. Baloch, H. Abro; Glyceryl trinitrate ointment in the treatment of anal fissures; JCPSP, 9 (1999), pp. 410–412
Document information
Published on 26/05/17
Submitted on 26/05/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?