(Created page with "==Abstract== Complex regional pain syndrome (CRPS) is a painful and disabling disorder that usually affects the extremities. This complication may affect the knee joint after...") |
m (Scipediacontent moved page Draft Content 820564591 to Ozcan-Soylev Boya 2016a) |
(No difference)
| |
Latest revision as of 10:07, 31 March 2017
Abstract
Complex regional pain syndrome (CRPS) is a painful and disabling disorder that usually affects the extremities. This complication may affect the knee joint after total knee arthroplasty (TKA). We report a unique case of CRPS of the foot and ankle, which was an unusual involvement site for CRPS after TKA.
Keywords
Complex regional pain syndromes ; Arthroplasty ; Replacement ; Knee ; Ankle ; Foot ; Complication
Introduction
Complex regional pain syndrome (CRPS) is a painful and disabling disorder that usually affects the extremities. The disease has two forms; symptoms occur without previous peripheral nerve injury in type 1 (Sudecks atrophy) and with previous injury to specific nerve in type 2.1 CRPS type 1 is usually initiated by some form of traumatic stimuli including injury and surgical intervention.1 ; 2
The pathophysiology of CRPS type 1 is not clear and many theories have been postulated.3
The disease has four cardinal features: pain, swelling, movement abnormalities, color–temperature-sudomotor changes.4 Pain is the most troubling complaint; it is not isolated to the area of injury or surgery and is out of proportion with the degree of injury.4 The diagnosis is excluded by the existence of any condition that would otherwise account for the degree of pain and dysfunction.5 ; 6
Total knee arthroplasty (TKA) surgery has many complications. It is also possible to observe TKA-related CRPS type 1 in the knee.7 ; 8 ; 9 Surgeons should suggest the disease (given certain findings) after TKA cases because treatment at the early stages is promising.6 ; 10 To the authors' knowledge, no cases of CRPS type 1 of the foot and ankle have been reported following TKA. We report a case of CRPS type 1 of the left foot and ankle following left TKA.
Case report
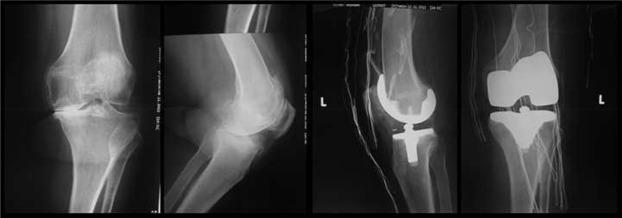
A 67-year-old woman was admitted to the outpatient clinic with complaints of left foot and ankle pain, swelling, limitation of motion and difficulty in weight bearing and walking. The patients history revealed a left TKA operation two months prior, and complaints started at the first month postoperatively (Fig. 1 ). Nonsteroidal anti-inflammatory drug (NSAID) failed to relieve the pain, swelling, and tenderness and these symptoms had gradually increased. The patient reported that she could not wear socks or shoes and could not walk without a cane due to pain. She described the pain as burning, numbness, and pins and needles sensations. Her sleep was also disturbed. The medical history of the patient included hypertension and a surgical procedure for cystocele.
|
|
|
Fig. 1. Preoperative and postoperative radiographs of the left knee. |
Physical examination of the patients left foot and ankle revealed non-dermatomal pain, swelling, edema over the dorsum of the foot and ankle, increased heat and redness, limitation of ankle motion (10° dorsiflexion and 40° plantar flexion) (Fig. 2 ). Moreover, allodynia, hyperesthesia and hyperalgesia were determined. However, muscle strength was normal and deep tendon reflexes were normoactive at left lower limb. The patients left ankle circumference was measured 2 cm larger compared to the right ankle. The calf was painless and Homans' sign was negative fort he left lower limb. Range of motion of the knee was nearly normal (0° extension, 100° flexion). There was no tenderness or pain at medial and lateral joint lines, patellofemoral joint, or retinaculi, as well as no swelling around the knee.
|
|
|
Fig. 2. Foot and ankle of the patient at presentation. |
Laboratory findings for the complete blood count, erythrocyte sedimentation rate, and C-reactive protein were normal. The serum rheumatoid factor was negative. Radiographs of the left foot and ankle showed a calcaneal spur. Mild soft tissue edema of the foot was observed on T2-weighted magnetic resonance images (MRI). Lumbar spine MRI revealed L4-5 right foraminal herniated disc, degenerative spondylosis, and chronic degenerative discopathy at multiple levels. According to the patients history, physical examination, laboratory results, and radiologic evaluation, the patient was diagnosed as CRPS type 1.
Operation report revealed that we have used tourniquet located midthight. Thus, there was no remarkably intra-operative blood loss. The tourniquet has inflated at 165 mm-Hg pressure and the pressure has kept along with the operation. Total tourniquet time was 105 min. Clinical reports revealed 520 ml visible blood loss via a hemovac drain and transfusion of two unites erythrocyte suspensions postoperatively. Also, there was no complication like infection or hematoma formation.
Amitriptyline 10 mg/day, pregabalin 150 mg/day, as well as vitamin C 1000 mg/day was prescribed. Additionally, the patient continued using previously prescribed NSAIDs. Elevation of the limb, retrograde massage and contrast bath therapy three times per day were recommended to produce desensitization and to reduce swelling. Passive and active range of motion exercises and mild stretching exercises were advised.
Swelling, increased heat, and redness subsided at the first month follow-up. Allodynia, hyperesthesia and hyperalgesia were reduced. There was nearly a full range of motion of the ankle. The patient reported that she could wear socks and shoes. At the last follow-up, at the end of the first year, the foot and ankle remained asymptomatic (Fig. 3 ).
|
|
|
Fig. 3. Foot and ankle of the patient at the end of the 1st year follow-up. |
Discussion
The onset of CRPS is usually precipitated by a physical injury; for example, a fracture, dislocation, sprain, or surgery.2 ; 11 ; 12 ; 13 Sometimes no particular cause can be found; in these cases, CRPS is defined as idiopathic.1
In the knee, also, its possible to diagnose CRPS type 1 after TKA cases.14 ; 15 Early references reported low incidence (%0.7–1.2) of CRPS type 1 after TKA, however, some reports have proposed that mild forms occur quite commonly after this operation.7 ; 8 ; 9 ; 16 A recent study reported high ratio of CRPS type 1 after TKA (%21 one month after operation and %12.7 after 6 months).17
Foot and ankle of the patient attacked by the disease, however, we have operated the patients ipsilateral knee. CRPS type 1 of foot after successful total hip arthroplasty previously reported.13 The patient was female and postmenopausal. CRPS is two- and four-fold more common in women, also, postmenopausal women appear to be at the highest risk of developing the condition.18 We identified the disease in a lower extremity, however, upper limbs most frequently involve.2 ; 18 ; 19 The disease usually presents within a month of injury and sometimes recognized at the second week following injury.20 ; 21 The complaints of the patient began during the fourth week of her postoperative period; these symptoms gradually increased.
Pain was the primary complaint of the patient. It was possible to produce hyperalgesia, allodynia with pin prick and non-noxious stimuli. In CRPS, pain is neuropathic in nature and is described as burning, aching, and throbbing.4 Swelling, joint stiffness, and vasomotor instability (color, temperature and sudomotor changes) are cardinal features of the condition; we observed these upon physical examination.4 The diagnosis for this condition is clinical; there is no diagnostic test.3 ; 4 The “Budapest criteria” are now recommended for diagnosis (Table 1 ).22 However, its sometimes difficult to use these criteria in clinical setting.4 It is possible to aid the diagnosis with other investigations. Routine laboratory tests can not be used to indicate CRPS.3 Plain radiographs demonstrate demineralization with patchy, subchondral or subperiostal osteoporosis, metaphyseal banding, and profound bone loss.3 ; 23 Of the cases, 30% show no radiographic change (similar to our case).4 Bone scanning in early stages reveals increased uptake and may return to normal, it is not specific but sensitive test.4 ; 10 ; 11 ; 24 MRI is not diagnostic but can be helpful to exclude other pathologies and in CRPS may demonstrate early bone and soft tissue edema, joint effusions and late atrophy with fibrosis.4 ; 10 ; 23 MRI of the patient revealed only mild soft tissue edema on the lateral side of the foot. Thermography, isolated cold stress testing, and sudomotor tests can also aid the diagnosis. These sensitive tests are not specific for CPRS.4 Thus, a clinical diagnosis remains the gold standard.10 ; 22
| At the time of examination the patient must report: | ||
| 1. Continuing pain | Disproportionate to inciting event | |
| 2. Symptoms | At least 1 in 3 of the following 4 categories: | |
| Sensory | Hyperesthesia/allodynia | |
| Vasomotor | Temperature/color changes-asymmetry | |
| Sudomotor | Oedema/sweating changes-asymmetry | |
| Motor/Trophic | Decreased ROM, weakness, tremor/dystonia Trophic changes in skin, hair or nails | |
| 3. Signs | At least 1 in 2 of the following categories: | |
| Sensory | Hyperaesthesia top in prick Allodyna to light touch | |
| Vasomotor | Evidence of temperature/colour asymmetry | |
| Sudomotor | Evidence of oedema/sweating asymmetry | |
| Motor/trophic | Tremotor/dystonia, trophic changes to skin, hair or nails | |
| 4. No other diagnosis explaining symptoms and signs | ||
The differential diagnosis of CRPS includes inflammatory arthritis, cellulites, osteomyelitis, deep vein thrombosis, chronic vascular disorders, diabetic neuropathy, entrapment neuropathies, and malignancy.23 We could exclude possible differential diagnosis with the aid of a clinical history and physical examination, radiographs, MRI, and laboratory tests. Pain characteristics (hyperalgesia and allodynia with non-noxious stimulus), physical examination findings (swelling, joint stiffness, and vasomotor instability [color, temperature and sudomotor changes]) were diagnostic for CRPS, also, clear laboratory–radiographs–MRI results assisted to exclude the diseases of differential diagnosis.
Most cases resolve (90% of CRPS symptoms resolve after two years), but a significant percentage do not.4 ; 21 If the disease progresses, the extremity becomes cold and the joint contractures appear. Its possible to observe trophic changes in late stages of the disease.3
Treatment of the disease is controversial.4 However, early treatment is thought to be beneficial.3 ; 6 ; 10 Functional capabilities may be affected due to CRPS if treatment is instituted in the later stages of the disease.6 The treatment options include physical therapies, medication and surgery. Elevation of the extremity, retrograde massage, contrast bath, desensitization training, fluidoteraphy, theuropathic ultrasound, whirlpool, transcutaneous electrical nerve stimulation, and physical/occupational therapy may be beneficial in CRPS.3 ; 25 ; 26 Calsitonin, bisphosphonates, corticosteroids, calcium channel blockers, capsaicin creams, and vitamin C have been found to be useful in acute CRPS.4 ; 27 Free radical scavengers such as Dimethyl Sulphoxide (DMSO) (topically administered) and N-Acetyl cysteine (orally administered) may be useful.4 ; 28 ; 29 Paracetamol and NSAIDs have not been proven to be beneficial.30 Gabapentin has been proven to be effective only in the first eight weeks of the disease.31 Tricyclic antidepressants can be used for the treatment of neuropathic pain.5 An intravenous regional guanethidine blockade does not help, and a meta-analysis does not support the use of a local anesthetic symphatic blockade.32 Surgical sympathectomy also has been used to improve symptoms.33 Amputation may be a treatment choice in patients with strongly resistant pain that will not be cured.34 Spinal cord stimulation is ineffective.35 We immediately began the treatment with amitriptyline and pregabalin. We also prescribed vitamin C for its antioxidant property.36 We observed dramatic response to the treatment at the fourth week of follow-up. However, resolution of the symptoms was achieved due to not only medical treatment but also other interventions such as retrograde massage, elevation, contrast bath therapy, and home exercise program.
Some reports suggest that complex regional pain syndrome type 1 may depend on in part tissue ischemia.37 Tourniquet ischemia may be responsible for the clinical picture; however, total tourniquet time was 105 min. In postoperative period, infection or hematoma formation may produce abnormal central sensitization and results in neuropathic pain.38 Conversely, we didn't encounter with infection or hematoma postoperatively.
In conclusion, CRPS type 1 of the foot and ankle is possible after TKA. Its important to keep this diagnosis in mind while managing a patient with painful foot and ankle after successful TKA. Early recognition and prompt initiation of treatment is so important for prognosis. Also, surgeons should mention the disease for whole lower limb in informed consent form regarding knee arthroplasty.
References
- 1 M. De Mos, M.C. Sturkenboom, F.J. Hugyen; Current understandings on complex regional pain syndrome; Pain Pract, 9 (2009), pp. 86–99
- 2 P.H. Veldman, H.M. Reynen, I.E. Arntz, R.J. Goris; Sings and symptoms of reflex sympathetic dystrophy: prospective study of 829 patients; Lancet, 342 (1993), pp. 1012–1016
- 3 G.S. Dowd, R. Hussein, V. Khanduja, A.J. Ordman; Complex regional pain syndrome with special emphasis on the knee; J Bone Jt Surg Br, 89 (2007), pp. 285–290
- 4 J. Field; Complex regional pain syndrome: a review; J Hand Surg Eur, 38 (2013), pp. 616–626
- 5 R.N. Harden; Pharmacotherapy of complex regional pain syndrome; Am J Phys Med Rehabil, 84 (2005), pp. S17–S28
- 6 S.M. Knoeller, M. Ehmer, B. Kleinmann, T. Wolter; CRPS I following artificial disc surgery: case report and review of literature; Eur Spine J, 20 (suppl 2) (2011), pp. S278–S283
- 7 A.W. Burns, D.A. Parker, M.R. Coolican, K. Rajoratnam; Complex regional pain syndrome complicating total knee arthroplasty; J Orthop Surg Hong Kong, 14 (2006), pp. 280–283
- 8 M.M. Katz, D.S. Hungerford, K.A. Krackow, D.W. Lennox; Reflex symphatic dystrophy as a cause of poor results after total knee arthroplasty; J Arthroplasty, 1 (1986), pp. 117–124
- 9 S. Nielsen, I. Hvid, O. Sneppen; Total condylar knee arthroplasty. A report of 2-year follow-up on 247 cases; Arch Orthop Trauma Surg, 104 (1985), pp. 227–232
- 10 M. Schürmann, G. Grandl, O. Rommel; Early diagnosis in post-traumatic complex regional pain syndrome; Orthopaedics, 30 (2007), pp. 450–456
- 11 M. de Mos, A.G.J. de Bruijn, F.J.P.M. Huygen, J.P. Dieleman, BHCh Stricer, M.C.J.M. Sturkenboom; The incidence of complex regional pain syndrome: a population-based study; Pain, 129 (2007), pp. 12–20
- 12 R. Mittal, R. Khetarpal, R. Malhotra, R. Kumar; The role of Tc-99 bone imaging in the management of pain after complicated total hip replacement; Clin Nucl Med, 22 (1997), pp. 593–595
- 13 M. Hossain, J.G. Andrew; Complex regional pain syndrome after hip replacement in a diabetic patient; Eur J Orthop Surg Traumatol, 20 (2010), pp. 501–503
- 14 D.E. Cooper, J.C. DeLee; Reflex symphatic dystrophy of the knee; J Am Acad Orthop Surg, 2 (1994), pp. 79–86
- 15 M.H. Gonzales, A.O. Mekhail; The failed total knee arthroplasty: evaluation and etiology; J Am Acad Orthop Surg, 12 (2004), pp. 436–446
- 16 R.M. Atkins; Complex regional pain syndrome; J Bone Jt Surg Br, 85 (2003), pp. 1100–1106
- 17 R.N. Harden, S. Bruehl, S. Stanos, V. Brander, O.Y. Chung, S. Saltz, A. Adams, S.D. Stulberg; Prospective examination of pain-related and psychological predictors of CRPS-like phenomena following total knee arthroplasty: a preliminary study; Pain, 106 (2003), pp. 393–400
- 18 G. Allen, B.S. Galer, L. Schwartz; Epidemiology of complex regional pain syndrome: a retrospective chart review of 134 patients; Pain, 80 (1999), pp. 539–544
- 19 I. Duman, U. Dincer, M.A. Taskaynatan, C. Cakar, I. Tugcu, K. Dincer; Reflex sympathetic dystrophy: a retrospective epidemiological study of 168 patients; Clin Rheumatol, 26 (2007), pp. 1433–1437
- 20 J. Field, R.M. Atkins; Algodystrophy is an early complication of Colles' fracture. What are the implications?; J Hand Surg Br, 22 (1997), pp. 178–182
- 21 A. Zyluk, P. Puchalski; Complex regional pain syndrome: observations on diagnosis, treatment and definition of new subgroup; J Hand Surg Eur Vol, 38 (2013), pp. 599–606
- 22 R.N. Harden, S. Bruehl, R.S. Perez, et al.; Validation of proposed diagnostic criteria (the “Budapest Criteria”) for complex regional pain syndrome; Pain, 150 (2010), pp. 268–274
- 23 A. Mc Bride, R. Atkins; Complex regional pain syndrome; Curr Orthop, 19 (2005), pp. 155–165
- 24 G.W. Lee, P.M. Weeks; The role of bone scintigraphy in diagnosing reflex symphatic dystrophy; J Hand Surg Am, 20 (1995), pp. 458–463
- 25 O.Y. Chung, S.P. Bruehl; Complex regional pain syndrome; Curr Treat Options Neurol, 5 (2003), pp. 499–511
- 26 K. Bengtson; Physical modalities for complex regional pain syndrome; Hand Clin, 13 (1997), pp. 443–454
- 27 D.D. Price, S. Long, B. Wilsey, A. Rafii; Analysis of peak magnitude and duration of analgesia produced by local anesthetics injected into sympathetic ganglia of complex regional pain syndrome; Clin J Pain, 14 (1998), pp. 216–226
- 28 J.H. Geertzen, H. de Bruijn, A.T. de Bruijn-Kofman, J.H. Arendzen; Reflex sympathetic dystrophy: early treatment and psychological aspects; Arch Phys Med Rehabil, 75 (1994), pp. 442–446
- 29 W.W. Zuurmond, P.N. Langendijk, P.D. Bezemer, H.E. Brink, J.J. de Lange, A.C. Van loenen; Treatment of acute reflex sympathetic dystrophy with DMSO 50% in a fatty cream; Acta Anaesthesiol Scand, 40 (1996), pp. 364–367
- 30 S.L. Collins, R.A. Moore, H.J. McQuay, P. Wiffen; Antidepressants and anticonvulsants for diabetic neuropathy and post herpetic neuralgia: a quantitative systematic review; J Pain Symptom Manage, 20 (2000), pp. 449–458
- 31 A.C. van de Vusse, S.G.M. Stomp-van den Berg, A.H.F. Kessels, W.E.J. Weber; Randomised control trial of Gabapentin in CRPS type 1 (ISTRCTN84121379); BMC Neurol, 4 (2004), p. 13 (29 September 2004)
- 32 M.S. Cepeda, J. Lau, D.B. Carr; Defining the therapeutic role of local anaesthetic sympathetic blockade in complex regional pain syndrome: a narrative and systematic review; Clin J Pain, 18 (2002), pp. 216–233
- 33 R.S. Perez, P.E. Zollinger, P.U. Dijkstra, et al.; The CRPS I task force. Evidence based guidelines for complex regional pain syndrome type 1; BMC Neurol, 10 (2010), p. 20 (31 March 2010)
- 34 P.W. Dielissen, A.T. Claassen, P.H. Veldman, R.J. Goris; Amputation for reflex sympathetic dystrophy; J Bone Jt Surg Br, 77 (1995), pp. 270–273
- 35 M.A. Kemler, H.C. de Vet, G.A. Barendse, F.A. van den Wildenberg, M. van Kleef; Effect of spinal cord stimulation for chronic complex regional pain syndrome type 1: five-year final follow-up of patients in a randomized controlled trial; J Neurosurg, 108 (2008), pp. 292–298
- 36 N. Shibuya, J.M. Humphers, M.R. Agarwal, D.C. Jupiter; Efficacy and safety of high-dose vitamin C on complex regional pain syndrome in extremity trauma and surgery-systematic review and meta-analysis; J Foot Ankle Surg, 52 (2013), pp. 62–66
- 37 T.J. Coderrea, D.N. Xanthos, L. Francisc, G.J. Bennett; Chronic post-ischemia pain (CPIP): a novel animal model of complex regional pain syndrome-type I (CRPS-I; reflex sympathetic dystrophy) produced by prolonged hindpaw ischemia and reperfusion in the rat; Pain, 112 (2004), pp. 94–105
- 38 M.J. Cousins, I. Power, G. Smith; 1996 Labat lecture: pain:a persistent problem; Reg Anesth Pain Med, 25 (2000), pp. 502–505
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?