(Created page with "==Abstract== ====Objectives==== The purpose of this study was to analyze the trends in cartilage repair strategies among Turkish orthopedic surgeons for isolated focal (oste...") |
m (Scipediacontent moved page Draft Content 524731425 to Elmali et al 2016a) |
(No difference)
| |
Latest revision as of 10:06, 31 March 2017
Abstract
Objectives
The purpose of this study was to analyze the trends in cartilage repair strategies among Turkish orthopedic surgeons for isolated focal (osteo)chondral lesions of the knee joint.
Materials and methods
A web-based survey of 21 questions consisting of surgical indications, techniques and time to return to sports was developed to investigate the preferences of members of the TOTBID and the TUSYAD.
Results
A total of 147 surgeons answered the questionnaire.70% of the respondents were TUSYAD members. 82% of respondents had at least five years experience in arthroscopy. Half of the surgeons indicated that patient age of 50 was the upper limit for cartilage repair. Irrespective of activity level, microfracture (60–67%) was the most frequently used technique for lesions smaller 2.5 cm2 . In lesions larger than 4 cm2 , MACI was the most commonly advocated procedure (67%). In patients with high activity levels, mosaicplasty was the first choice (69%) for lesions between 2.5 and 4 cm2 in size, followed by MACI (27%).
Conclusion
Patient age, activity level, BMI and lesion size were important determinants for the choice of treatment of isolated chondral lesions in the knee. These results reflect the choices of experienced knee surgeons in the country. Although not widely performed in Turkey and has limited reimbursement by the health care system, the first choice for defects over 4 cm2 was second generation ACI. Third party payers & health reimbursement authorities should take into account that large defects require methods which are relatively expensive and need high technology. Cross-sectional survey, Level II.
Keywords
Cartilage ; Survey ; Turkey ; Cartilage repair ; Knee ; Osteochondral lesion ; Web-based-survey ; Microfracture ; Mosaicplasty ; Autologous chondrocyte implantation
Introduction
Injuries to the articular cartilage of the knee are common. Due to its inherent lack of vascular supply and limited intrinsic regeneration capacity of articular cartilage, untreated cartilage defects may lead to early onset osteoarthritis. The management of symptomatic focal traumatic articular cartilage lesions of the knee in active individuals remains a substantial challenge. Although a variety of methods have the potential to stimulate the formation of a new articular surface, none of the current techniques including microfracture, autologous or allogenic osteochondral grafts, autologous chondrocyte implantation (ACI), growth factors and scaffolds are able to replicate the original anatomy and architecture of hyaline cartilage.1 ; 2 Choosing the best technique that addresses the individual defect is a challenge for the orthopedic surgeon. Smaller defects not affecting the subchondral bone are usually treated with microfracturing while lesions with loss of subchondral bone can be managed with autologous osteochondral autograft transfer (OAT) ie. mosaicplasty. Defects larger than 2.5 cm2 , can still be managed with microfracture and OAT however, their limited effectiveness in larger lesions has led the search for advanced cartilage repair strategies such as matrix-assisted chondrocyte implantation (MACI).
There is no universally accepted algorithm for treatment of cartilage defects and the treatment preferences of Turkish orthopedic surgeons are not known. The goal of this study was to analyze the treatment preferences of Turkish orthopedic surgeons for different types of cartilage defects and to potentially highlight treatment recommendations.
Material and methods
A 21-item electronic questionnaire prepared by the members of the TUSYAD Cartilage Committee was designed to collect data on indications for surgery, patient characteristics (including patient age, BMI, activity level) and treatment options to evaluate the cartilage repair practice patterns of Turkish orthopedic surgeons (Table 1 shows first 16 questions). This survey was performed on Turkish Society of Orthopedics & Traumatology (TOTBID) and Turkish Society of Sports Injuries, Arthroscopy & Knee Surgery (TUSYAD) members. The survey was completed via the web using Survey Monkey (http://www.surveymonkey.com ). The ICRS (International Cartilage Repair Society) Classification for focal cartilage lesion was used to define cartilage defects.3
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Results
Surgeon demographics
A total of 147 surgeon members of TOTBID filled out the questionnaire. Ninety eight (70%) of the responders were also members of TUSYAD. Approximately 1/3 of the respondents practiced in a private hospital, 1/3 in a university clinic, 15% in a state hospital and 13% in a state teaching and research hospital. Seventy nine percent of the respondents performed knee arthroscopy as the most frequent procedure. This was followed by arthroplasty (48%) & trauma surgery (42%). Most of the surgeons had more than 5 years experience in knee surgery and performed more than 50 arthroscopic procedures per year. The majority of the surgeons treated cartilage defects in the knee and ankle joints arthroscopically, arthroscopic treatment of shoulder cartilage defects were less frequent (Table 2 ).
| Year of practice in knee surgery | Percentage (%) |
|---|---|
| 0–5 years | 16 |
| 6–10 years | 22 |
| 11–20 years | 39 |
| 21 (+) years | 21 |
| Number of arthroscopies per year | |
| 50 (−) | 20 |
| 51–100 | 40 |
| 101–200 | 24 |
| 201 (+) | 17 |
| Joints treated arthroscopically | |
| Knee | 87 |
| Ankle | 67 |
| Shoulder | 18 |
| All 3 joints | 12 |
Conservative treatment
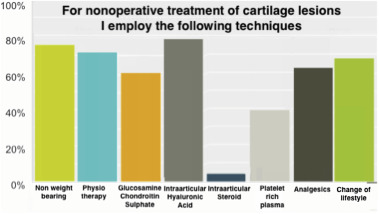
The most common non-surgical treatment offered by the respondents were intra-articular hyaluronic acid injections (80%) and physiotherapy (75%). This was followed by lifestyle changes (70%), systemic pain medication (65%), oral glucosamine (60%) and platelet rich plasma injections (41%). The rate of surgeons using steroid injections was only 5,6% (Fig. 1 ).
|
|
|
Fig. 1. Rate of non-surgical treatment modalities employed by the respondents. |
Surgical treatment
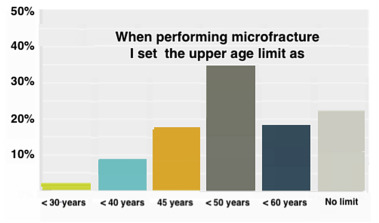
The upper age limit for cartilage surgery was reported as 50 years by 52%, 40 years by 25% of the surgeons and 60 years by 12%. Obesity was also an important factor in deciding surgical treatment. The upper limit of body mass index (BMI)was accepted as 30 kg/m2 by 58% and 25 kg/m2 by 22% of the respondents. Location of the cartilage defect had a significant effect on the outcome. The best results were obtained in the lesions of the femoral condyles (85% of the surgeons). The most commonly performed cartilage procedure was microfracture (60–80%) followed by mosaicplasty (20–40%). MACI was utilized by less than 10% of the surgeons. A third of the surgeons performing microfracture accepted the upper age limit as 50. Seventeen percent lowered this limit to 45 while twenty-three percent of the surgeons thought that age was not an important factor (Fig. 2 ). Microfracture was performed using a dedicated instrument by 81% of the surgeons. More than half of the surgeons (58%) did not use a continuous passive motion device (CPM) after surgery. The most common usage was reported to be 2 h/day in the first week for respondents who used a CPM device (27%). Partial weight bearing after microfracture was allowed in 4 weeks by 23% of the surgeons, while for 22% this time period extended to 6 weeks. Twenty five percent of the respondents allowed full weight bearing on the 6th post-operative week. Time to return to sports following cartilage repair was advocated at 6 months for microfracture (86%), 9 months for mosaicplasty (63%), and 12 months for MACI (73%) (18 question).
|
|
|
Fig. 2. For microfracture, the upper age limit accepted by surgeons. |
Lesion size & depth
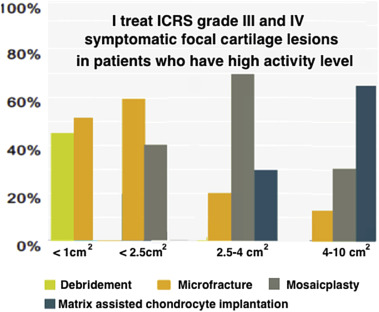
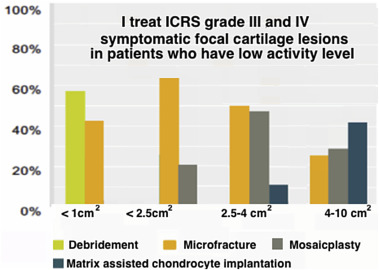
In patients with high activity levels, ICRS grade 3–4 lesions smaller than 2.5 cm2 , were most frequently treated with microfracture (60%) followed by mosaicplasty (40%). For mid-size lesions between 2.5 and 4 cm2 , mosaicplasty was the first option (%69), followed by MACI (%27). In lesions larger than 4 cm2 , MACI was the most commonly advocated procedure (%67). Ninety percent of the surgeons had never used scaffold augmented microfracture but 17% would consider its use in active patients under 45 years of age (Fig. 3 ). In patients with low activity levels, ICRS grade 3–4 lesions smaller than 2.5 cm2 were most frequently treated with microfracture (67%) followed by mosaicplasty (23%). For mid-size lesions between 2.5 and 4 cm2 , microfracture was still the first option in 54% followed by mosaicplasty in %69. In lesions larger than 4 cm2 , MACI was the most commonly advocated procedure (%38), followed by mosaicplasty in 30% and microfracture in 28% (Fig. 4 ). Fifty percent of the surgeons would not offer surgical treatment for symptomatic ICRS grade 1–2 lesions smaller than 1 cm2 but would consider surgery in larger lesions. The preferred operative treatment of ICRS grade 1–2 lesions between 1 and 4 cm2 was debridement in 53%, antegrade or retrograde drilling was the second choice. For cartilage lesions involving the subchondral bone, 42.4% of the surgeons would address both bone and cartilage defects. This would involve a one stage operation in 25.4% while a two stage operation would be advised in a significantly less number of cases (7.6%). Only 13% of the surgeons would prefer microfracturing to treat such lesions, while a total of 28.8% would utilize either an osteochondral plug or bone grafting + ACI depending on lesion size.
|
|
|
Fig. 3. Treatment preferences for athletes with high activity levels who have a symptomatic cartilage lesion (Answers for question 19). |
|
|
|
Fig. 4. Treatment preferences for athletes with low activity level who have symptomatic cartilage lesion (Answers for question 20). |
Discussion
Several important trends have emerged from the findings of this study. Mosaicplasty or ACI was the first choice in high activity patients for mid sized (2,5–4 cm2 ) defects. This may be due to the progressive deterioration of the outcomes of microfracture over the years and implies the need for a more durable treatment in these cases. Although limitations for reimbursement & cost are important issues, MACI was the first choice for larger defects (over 4 cm2 ). Third party payers & health authorities should consider this need for advanced cartilage regeneration techniques and should implement the necessary regulations and reimbursement systems to make these treatments available to orthopedic surgeons. It is interesting to note that, although cell free scaffolds were available, 90% of the surgeons had never used this technique at the time of the study. This may be explained by the limited evidence for the efficacy of these cell free implants.
Despite the fact that there have been a variety of methods for cartilage repair, to date, no universally accepted treatment guidelines concerning patient age, lesion size, depth (chondral/osteochondral), rehabilitation or return to sports exist.4 Unfortunately, no clear recommendations have emerged from well designed, randomized-controlled trials for the treatment of focal cartilage defects.5 ; 6 ; 7 ; 8 The aim of this survey was to analyze the preferences for treatment of focal knee cartilage defects among a community of experienced musculoskeletal surgeons. The findings of the study reflect the preferences of experienced and active knee surgeons in the country as 84% had been in practice more than 5 years. 80% performed more than 50 arthroscopic procedures per year. This survey of experienced surgeons may help to identify the most appropriate and current treatment methods until studies with higher levels of evidence can be performed.
Numerous agents for the conservative treatment of chondral lesions and early osteoarthritis.9 ; 10 ; 11 In this survey, the most frequently used conservative measures were intra-articular hyaluronic acid injections and physiotherapy. These were followed by lifestyle changes and systemic pain medication and glucosamine/chondroitin sulfate supplements. Less than half of the surgeons used platelet rich plasma injections despite the hype and media pressure surrounding its use. Although preliminary studies describe symptomatic benefit of PRP injections for a limited time period; more studies are needed to clarify the role of different methods of production, PRP characteristics, presence and absence of leukocytes, clinical indications, way of administration and therapeutic protocols.12 Although widely used by the rheumatologists, the ratio of surgeons who used steroid injections was only 5,6%. This may be due to its limited and short term benefit on pain and function.11
Various surgical techniques, both reparative and regenerative, have been used to treat focal (osteo) chondral pathology.13 ; 14 ; 15 Since Steadman first described its use in the 1980s, microfracture has become popular as a first-line treatment for chondral injuries.16 ; 17 The clinical outcome seems dependent on the patients age, level of activity, defect location and postoperative regimen.16 ; 17 The underlying principle of the microfracture technique is bone marrow stimulation and penetration of the subchondral bone plate resulting in the recruitment of mesenchymal stem cells which eventually differentiate into fibrocartilage.5 ; 6 ; 17 ; 18 ; 19 ; 20 ; 21 ; 22 ; 23 ; 24 ; 25 ; 26 Although the initial results of microfracture are satisfactory in 80% of the patients, the regenerate is mainly composed of fibrocartilage and the results begin to deteriorate over time after 4–5 years.5 ; 6 ; 24 ; 26 In our survey, microfracture was found to be the most common cartilage repair procedure (60–80%) followed by mosaicplasty in 20–40%. MACI was performed by less than 10% of the surgeons. Many studies have shown that younger age and smaller lesions results in better outcomes following microfracture.5 ; 6 ; 17 ; 18 ; 19 ; 20 ; 21 ; 22 ; 23 ; 24 ; 25 ; 26 While microfracture gives best results in patients under the age of 40 years, an upper age limit beyond which microfracture confers little or no benefit has not been established. In this survey, 23% of surgeons indicated that they had no upper age limit for performing microfracture, while 34% indicated an upper age limit of 50 years. This over utilization of microfracture may be due to the limited availability of other cartilage repair techniques due to reimbursement and regulatory issues. In patients with high activity level, lesions smaller than 2.5 cm2 , were most frequently treated with microfracture followed by mosaicplasty. This was reversed for mid size lesions between 2.5 and 4 cm2 where mosaicplasty was the treatment of choice. Mosaicplasty is perceived as a more durable solution that achieves a covering of hyaline cartilage in these active patients. Comparative studies have shown higher activity levels and better clinical results after mosaicplasty compared to microfracture.18 ; 27 However the utilization of mosaicplasty is limited by the size of the donor area. Donor site symptoms, although reported to be less than 5%, are also an important issue.28 This has led to search for alternative solutions in larger defects over 4 cm2 . MACI has is an attractive option in these cases as the technique is not limited by the size and shape of the defect.22 ; 24 ; 29 ; 30 Regulatory and reimbursement issues, the need for two stage surgery and expense are the main issues preventing widespread use of MACI. The first choice for large defects was MACI in this survey although less than 10% of the surgeons had performed the technique. This underscores the demand for advanced cartilage repair techniques in these rare but potentially debilitating cartilage lesions. The current regulations in Turkey severely limit the use of MACI and reimbursement is only possible in a select group of hospitals after pre-approval of the Ministry of Health. Third party payers still consider MACI as an experimental procedure although the technique has been in use for more than two decades and its efficacy has been demonstrated in over 20.000 patients treated with either 1st generation ACI or MACI.29 ; 30 Third party payers should be aware of the need for advanced (albeit expensive) technologies for larger chondral defects. Microfracture was the most commonly preferred technique in small and mid-sized lesions in patients with low activity levels. MACI (48%) was the first choice in larger defects, although mosaicplasty (30%) & microfracture (25%) were also considered.
In our survey, body mass index (BMI) was considered an important factor in decision making by 84% of the respondents. The upper limit of cartilage regeneration surgery was stated as below 30 kg/m2 by 58%. A BMI larger than 30 kg/m2 has been correlated with an inferior outcome after microfracture and cartilage procedures.17 ; 20 Hence, it would certainly seem logical to establish a BMI value beyond which microfracture should not be attempted.
The postoperative regimen after microfracture remains one of the most debated issues regarding this technique. CPM has been shown to improve the quality of regenerated cartilage in the experimental setting.31 However, no randomized, controlled studies have studied the beneficial effects of CPM in humans after microfracture.17 ; 18 ; 21 ; 25 In our survey, more than half of the respondents did not use CPM in the rehabilitation phase. This might be due to constraints of expense and availability of home CPM devices. Those who used CPM after surgery most frequently recommended 2 h per day in the first weeks. The recommended 6 weeks therapy could not be completed for most of the cases, this again is probably due to logistical problems and expense. Weight bearing after microfracture is another debated issue. The survey questions did not specify the size or location of the lesion, therefore a variety of answers were obtained. Partial weight bearing was allowed at 2 weeks by 13%, 4 weeks by 23%, 6 weeks by 22% of the respondents. Similarly full weight bearing was allowed at 2 weeks 6%, 4 weeks 9%, 6 weeks by 25% of the respondents. This indicates that the respondents adopted a conservative and restricted weight bearing regimen after surgery. Return to active sports following cartilage repair was accepted at 6 months for microfracture (86%), 9 months for mosaicplasty (63%), and 12 months for MACI (73%). This is in contrast to several studies in the literature which have found earlier return to sports after mosaicplasty compared to microfracture.18 ; 27 ; 32 The late return to sports after ACI is expected as these are complex cases and the desire of the surgeons to wait for maturation of the regenerate.
Although 90% of surgeons had never use the matrix-supported microfracture method, 17% considered that it could be a choice for individuals with a high activity level and younger than 45 years. This underscores the need for newer and innovative techniques based on the unsatisfactory results of microfracture.
In conclusion, this study gives important information on the trends of cartilage repair of Turkish orthopedic surgeons. Third party payers should take into account the need for advanced and probably more expensive cartilage repair technologies since current techniques have unsatisfactory outcomes in larger lesions and younger active patients.
References
- 1 J. Farr, B.J. Cole, A. Dhawan, J. Kercher, S. Sherman; Clinical cartilage restoration: evolution and overview; Clin Orthop Relat Res, 469 (2011), pp. 2696–2705
- 2 J.A. Buckwalter; Evaluating methods for restoring cartilaginous articular surfaces; Clin Orthop Relat Res, 367S (1999), pp. S224–S238
- 3 M. Brittberg, C.S. Winalski; Evaluation of cartilage injuries and repair; J Bone Jt Surg Am, 85-A (Suppl. 2) (2003), pp. 58–69
- 4 R.B. Jakobsen, L. Engebretsen, J.R. Slauterbeck; An analysis of the quality of cartilage repair studies; J Bone Jt Surg Am, 87 (2005), pp. 2232–2239
- 5 G. Knutsen, J.O. Drogset, L. Engebretsen, et al.; A randomized trial comparing autologous chondrocyte implantation with microfracture: findings at five years; J Bone Jt Surg Am, 89 (2007), pp. 2105–2112
- 6 G. Knutsen, L. Engebretsen, T.C. Ludvigsen, et al.; Autologous chondrocyte implantation compared with microfracture in the knee: a randomized trial; J Bone Jt Surg Am, 86-A (2004), pp. 455–464
- 7 J.P. Benthien, M. Schwaninger, P. Behrens; We do not have evidence based methods for the treatment of cartilage defects in the knee; Knee Surg Sports Traumatol Arthrosc, 19 (4) (2011), pp. 543–552
- 8 J. Theodoropoulos, T. Dwyer, D. Whelan, P. Marks, M. Hurtig, P. Sharma; Microfracture for knee chondral defects: a survey of surgical practice among Canadian orthopedic surgeons; Knee Surg Sports Traumatol Arthrosc, 20 (2012), pp. 2430–2437
- 9 P. Jüni, S. Reichenbach, S. Trelle, et al.; Efficacy and safety of intra-articular hylan or hyaluronic acids for osteoarthritis of the knee: a randomized controlled trial; Arthritis Rheum, 56 (11) (2007), pp. 3610–3619 9
- 10 D.O. Clegg, D.J. Reda, C.L. Harris, et al.; Glucosamine, chondroityn sulfate, and the two in cambination for painful knee osteoarthritis N; Engl J Med, 354 (8) (2006), pp. 795–808
- 11 N. Bellamy, J. Campbell, V. Robinson, T. Gee, R. Bourne, G. Wells; Intra-articular corticosteroid for treatment of osteoarthritis of the knee; Cochrane Database Syst Rev, 19 (2) (2006), p. CD005328 submitted for publication
- 12 S. Zaffagnini, G. Filardo, E. Kon, et al.; The treatment of large degenerative defects; M. Brittberg, A. Imhoff, H. Madry, M. Mandelbaum (Eds.), Cartilage Repair. Current Concepts (2010), pp. 89–98
- 13 J.E. Bekkers, M. Inklaar, D.B. Saris; Treatment selection in articular cartilage lesions of the knee: a systematic review; Am J Sports Med, 37 (Suppl. 1) (2009), pp. 148S–155S
- 14 T.S. de Windt, J.E. Bekkers, L.B. Creemers, W.J. Dhert, D.B. Saris; Patient profiling in cartilage regeneration: prognostic factors determining success of treatment for cartilage defects; Am J Sports Med, 37 (Suppl. 1) (2009), pp. 58S–62S
- 15 J.D. Harris, R.H. Brophy, R.A. Siston, D.C. Flanigan; Treatment of chondral defects in the athletes knee; Arthroscopy, 26 (2010), pp. 841–852
- 16 M. Asik, F. Ciftci, C. Sen, M. Erdil, A. Atalar; The microfracture technique for the treatment of full-thickness articular cartilage lesions of the knee: midterm results; Arthroscopy, 24 (2008), pp. 1214–1220
- 17 R.J. Williams 3rd, H.W. Harnly; Microfracture: indications, technique, and results; Instr Course Lect, 56 (2007), pp. 419–428
- 18 R. Gudas, R.J. Kalesinskas, V. Kimtys, et al.; A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes; Arthroscopy, 21 (9) (2005), pp. 1066–1075
- 19 P.C. Kreuz, M.R. Steinwachs, C. Erggelet, et al.; Results after microfracture of fullthickness chondral defects in different compartments in the knee; Osteoarthr Cartil, 14 (2006), pp. 1119–1125
- 20 K. Mithoefer, R.J. Williams 3rd, R.F. Warren, et al.; The microfracture technique for the treatment of articular cartilage lesions in the knee: a prospective cohort study; J Bone Jt Surg Am, 87 (2005), pp. 1911–1920
- 21 J.R. Steadman, W.G. Rodkey, J.J. Rodrigo; Microfracture: surgical technique and rehabilitation to treat chondral defects; Clin Orthop Relat Res, 391 (Suppl.) (2001), pp. S362–S369
- 22 E. Kon, G. Filardo, M. Berruto, et al.; Articular cartilage treatment in high-level male soccer players: a prospective comparative study of arthroscopic second-generation autologous chondrocyte implantation versus microfracture; Am J Med, 39 (12) (2011), pp. 2549–2557
- 23 J.R. Steadman, K.K. Briggs, J.J. Rodrigo, M.S. Kocher, T.J. Gill, W.G. Rodkey; Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up; Arthroscopy, 19 (2003), pp. 477–484
- 24 D.B. Saris, J. Vanlauwe, J. Victor, et al.; Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture; Am J Sports Med, 37 (Suppl. 1) (2009), pp. 10S–19S
- 25 K. Mithoefer, T. McAdams, R.J. Williams, P.C. Kreuz, B.R. Mandelbaum; Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis; Am J Sports Med, 37 (10) (2009), pp. 2053–2063
- 26 K. Mithoefer, K. Hambly, S. Della Villa, H. Silvers, B.R. Mandelbaum; Return to sports participation after articular cartilage repair in the knee: scientific evidence; Am J Sports Med, 37 (Suppl. 1) (2009), pp. 167S–176S
- 27 A.J. Krych, H.W. Harnly, S.A. Rodeo, R.J. Williams 3rd; Activity levels are higher after osteochondral autograft transfer mosaicplasty than after microfracture for articular cartilage defects of the knee: a retrospective comparative study; J Bone Jt Surg Am, 94 (11) (2012), pp. 971–978
- 28 G.A. Matricali, G.P. Dereymaeker, F.P. Luyten; Donor site morbidity after articular cartilage repair procedures : a review; Acta Orthop Belg, 76 (5) (2010), pp. 669–674
- 29 S.P. Krishnan, J.A. Skinner, W. Bartlett, et al.; Who is the ideal candidate for autologous chondrocyte implantation?; J Bone Jt Surg Br, 88 (2006), pp. 61–64
- 30 D.B. Saris, J. Vanlauwe, J. Victor, et al.; Characterized chondrocyte implantation results in better structural repair when treating symptomatic cartilage defects of the knee in a randomized controlled trial versus microfracture; Am J Sports Med, 36 (2) (2008), pp. 235–246
- 31 J.M. Williams, M. Moran, E.J. Thonar, R.B. Salter; Continuous passive motion stimulates repair of rabbit knee articular cartilage after matrix proteoglycan loss; Clin Orthop Relat Res, 304 (1994), pp. 252–262
- 32 L. Hangody, J. Dobos, E. Balo, G. Panics, L.R. Hangody, I. Berkes; Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17-year prospective multicenter study; Am J Sports Med, 38 (6) (2010), pp. 1125–1133
Document information
Published on 31/03/17
Licence: Other
Share this document
Keywords
claim authorship
Are you one of the authors of this document?